MODE OF ACTION
progress through the inflammatory
phase of healing, stimulating cellular
proliferation and allowing granulation
to occur.
Analysis of wound exudate
collected in canisters following
NPWT has been shown to contain
exudate-associated proteases and
cytokines, which demonstrates that
they can be removed from a wound
with NPWT; while tissue biopsies
and serum analysis of NPWT-treated
wounds have shown a reduction
in inflammatory infiltrate and a
modulation of cytokines, resulting in
reduced inflammation (Stechmiller et
al, 2006; Mouës et al, 2008).
The presence of inflammation
in chronic wounds leads to a rise in
capillary permeability and an increase
in interstitial fluid, both of which result
in tissue oedema. Oedema compresses
local capillaries and increases the
distance between capillaries, thereby
limiting the supply of oxygen and
nutrients to tissues. Reducing oedema
is widely reported to be a key mode
of action in NPWT,
particularly in
closed incisions
following surgery.
However, clinical
or experimental
evidence to
support this theory
is limited due to the
difficulty in measuring
oedema. The application of
mechanical forces (in this
case NPWT) to wound tissue
may improve oedema either
by directly removing excessive
interstitial fluid or preventing
further leakage from the
capillaries through the application
of compressive force — it is also
possible that the enhanced drainage of
interstitial fluid through the lymphatic
system plays a role (Kilpadi and
Cunningham, 2011).
Maintenance of homeostasis
The role of NPWT as a closed system
is often underestimated, but it
contributes to a micro-environment
that is conducive to wound healing.
Moisture balance is important across
all phases of wound healing — too
little moisture can cause cell death
and tissue necrosis, whereas too
settings, irrespective of the simplicity
or complexity of the source of the
vacuum, the type of wound filler or the
level of pressure applied (Armstrong
et al, 2012; Dorafshar et al, 2012;
Rahmanian-Schwarz et al, 2012).
Such studies continue to challenge
some of the assumptions that have
surrounded NPWT for so long and are
beginning to reinforce the notion that
NPWT can offer clinicians a flexible
yet effective approach to managing
wounds, in particular by paying closer
attention to the needs of their patients.
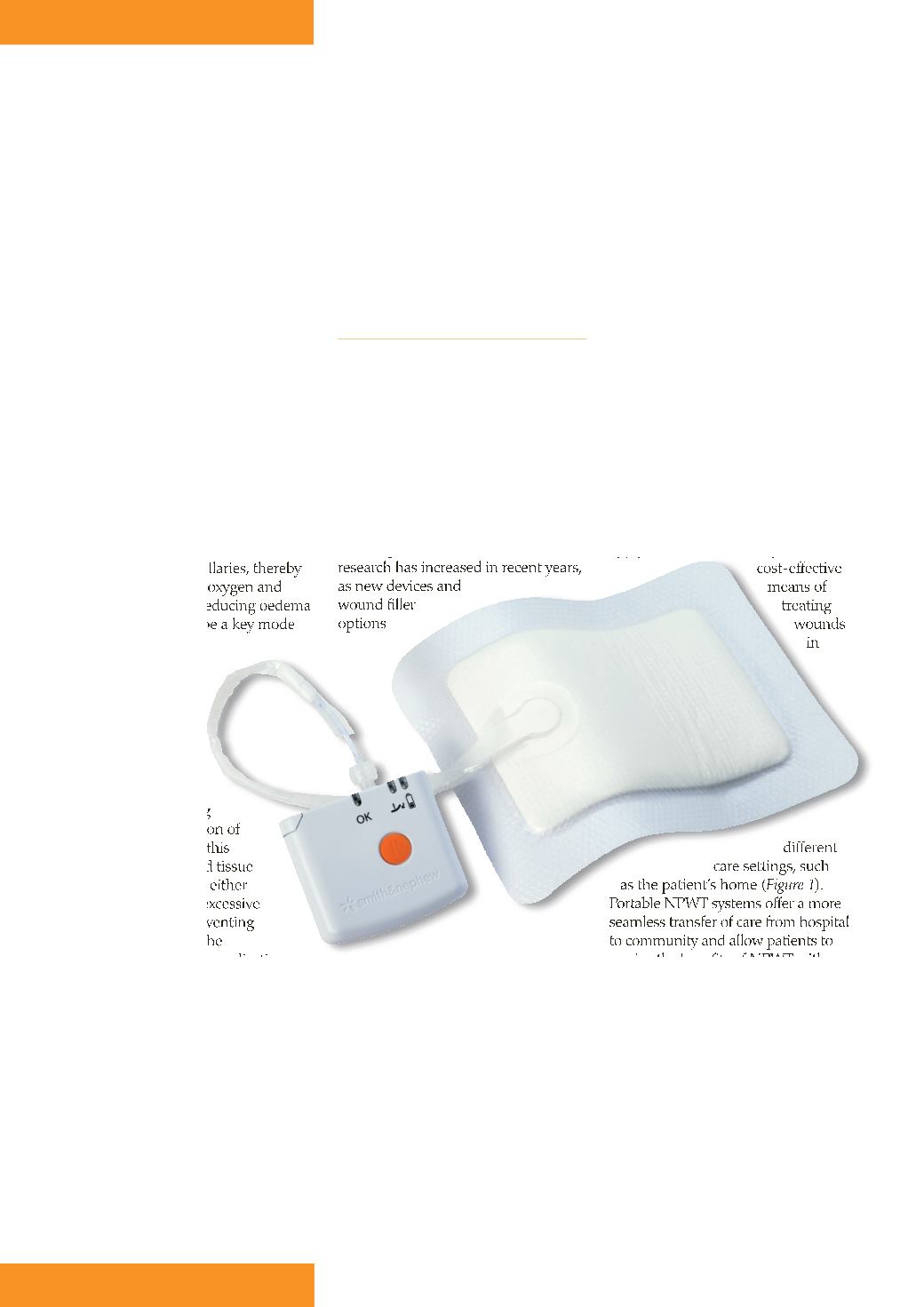
Portable NPWT systems
Recent developments in NPWT
technology have led to the
introduction of single-use NPWT
systems, which are smaller, more
portable (they can be worn on the
person rather than carrying a large
heavy device), simpler to use and
apply,
and provide a
cost-effective
means of
treating
wounds
in
different
care settings, such
as the patient’s home (
Figure 1
).
Portable NPWT systems offer a more
seamless transfer of care from hospital
to community and allow patients to
receive the benefits of NPWT with
minimal impact on daily living.
With respect to NPWT’s key modes
of action, experimental studies have
demonstrated that single-use NPWT
units function in the same manner
as larger, traditional NPWT devices
(Malmsjö et al, 2014). Similarly,
clinical studies have shown that
single-use systems offer equivalent
clinical outcomes to traditional NPWT
devices. For instance, Armstrong et
al (2012) compared an ultraportable
single-use NPWT system with
traditional NPWT in 132 patients
much results in maceration to the
surrounding tissue. A closed system
also minimises the likelihood of
wound contamination from the
external environment. The fact that
NPWT requires fewer dressing
changes than traditional wound care
practices (Hurd et al, 2014) further
minimises disruption to the wound’s
homeostasis and/or exposure to
external contamination.
CONSIDER NPWT CHOICES
It is clear from the evidence that there
are multiple mechanisms of action
associated with NPWT, many of which
are interrelated. However, the body of
knowledge around these mechanisms
has remained largely the same
since the first experimental studies
were published almost 20 years ago
(Morykwas et al, 1997).
The publication of NPWT-related
research has increased in recent years,
as new devices and
wound filler
options
become available and clinicians and
manufacturers begin to question
the accepted principles of NPWT
treatment in areas such as optimum
pressure levels, pressure modalities
(continuous or intermittent), optimum
filler materials, and pump choice.
Recently published randomised
controlled trials (RCTs) comparing
different systems suggest that NPWT
is consistently effective across a
variety of wound types and care
8
JCN supplement
2015,Vol 29, No 5
Figure 1.
Portable NPWT system.









