WOUND CHRONICITY
›
JCN supplement
2015,Vol 29, No 5
5
healing may take longer because
diagnosis and treatment choice is not
adequate. A study by Dowsett et al
(2014) revealed that of 1,166 wounds
managed across eight community
settings, 26.4% of wounds had been
present for over six months, and
16.5% over one year.Wounds of a long
duration increase the risk of infection
and other complications, presenting
a considerable burden on both the
healthcare system and patient.
MANAGEMENT
Most chronic wounds can be
encouraged to heal by removing
underlying barriers to healing, such as
improving nutrition and controlling
underlying medical conditions. The
wound bed can then be prepared for
healing. If these factors are addressed
and there is no improvement, further
intervention may be required.
FUTURE OF CHRONIC WOUNDS
IN THE COMMUNITY
Nurses carry out the majority
of chronic wound care in the
community setting. As the number
of patients with chronic wounds
is set to increase over the coming
years, healthcare providers need to
look closely at optimising the future
delivery of care (Dowsett et al, 2014;
Hampton, 2015).
REFERENCES
Department of Health (2009)
NHS 2010–2015:
from good to great. Preventative, people-centred,
productive
. DH, London
Dowsett C, Bielby A, Dearle R (2014)
Reconciling increasing wound care demands
with available resources.
J Wound Care
23(11):
552–62
Drew P, Posnett J, Rusling L, Wound Care Audit
Team (2007) The cost of wound care for a
local population in England.
Int Wound J
4(2):
149–55
Eagle M (2009) Wound assessment: the patient
and the wound.
Wound Essentials
4:
14–24
Gottrup F, Henneberg E, Trangbæk R,
Bækmark N, Zøllner K, Sørensen J (2013)
Point prevalence of wounds and cost impact
in the acute and community settings in
Denmark.
J Wound Care
22(8): 413–4, 416,
418–22
Griffiths P ((2010) How good is the evidence
for using risk assessment to prevent pressure
ulcers?
Nurs Times
106(14):
10–13
Hampton J (2015) Providing cost-effective
treatment of hard-to-heal wounds in the
community through NPWT.
Br J Community
Nurs
20(sup 6):
S14–S20
Ovington LG, Schultz GS (2004) The
physiology of wound healing. In:
Chronic
Wound Care: A Problem-based Learning
approach
. 83–99
Posnett J, Franks P (2007)
The cost of skin
breakdown and ulceration in the UK
. The
Smith and Nephew Foundation, Hul
Posnett J, Gottrup F, Lundgren H, Saal G
(2009) The resource impact of wounds on
healthcare providers in Europe.
J Wound Care
18(4):
154–61
Shipperley T, Martin C (2002) The physiology
of wound healing: an emergency response.
NT Plus, Wound Care
98:
8
Stephen-Haynes J, Hampton S (2010)
Achieving Effective Outcomes in Patients
with Overgranulation.
WCAUK Education,
Droitwich
Timmons J (2006) Factors adversely
influencing wound healing. In: Gray D,
Cooper P, Timmons J (2006)
Essential
Wound Management: An Introduction for
Undergraduates
. Wounds UK, Aberdeen:
47–71
Upton D, Hender C, Solowiej K (2012) Mood
disorders in patients with acute and chronic
wounds: a health professional perspective.
J
Wound Care
21(1):
42–8
Vowden K,Vowden P (2004) The role
of exudate in the healing process. In:
Understanding Exudate Management
. White
RJ, ed. Trends in Wound Care,Volume III.
Quay books, MA Healthcare Ltd, London
Werdin F, Tennenhaus M, Schaller H,
Rennekampff H (2009) Evidence-based
management strategies for treatment of
chronic wounds.
Eplasty
9: e19
Younes N, Albsoul A, Badran D, Obedi S (2006)
Wound bed preparation with 10 percent
phenytoin ointment increases the take of
split-thickness skin graft in large diabetic
ulcers.
Dermat Online J
12(6): 5
Common chronic wound types seen in the community
The most commonly encountered chronic wounds in the community setting are leg ulcers,
diabetic foot ulcers and pressure ulcers (Drew et al, 2007).
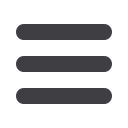
LEG ULCERS
Venous leg ulceration is a result of underlying venous disease. It is estimated
that between 70,000–190,000 people in the UK have an open ulcer at any time
(Posnett and Franks, 2007). These wounds can have a negative impact on
patient wellbeing by causing pain, odour, stress, low self-esteem and even
depression (Upton et al, 2012).
DIABETIC FOOT ULCERS
These usually occur over bony prominences, with sloughy and/or necrotic
tissue. They have a high risk of complications (and can result in amputations
if not treated promptly and appropriately). Amultidisciplinary team
approach is required.
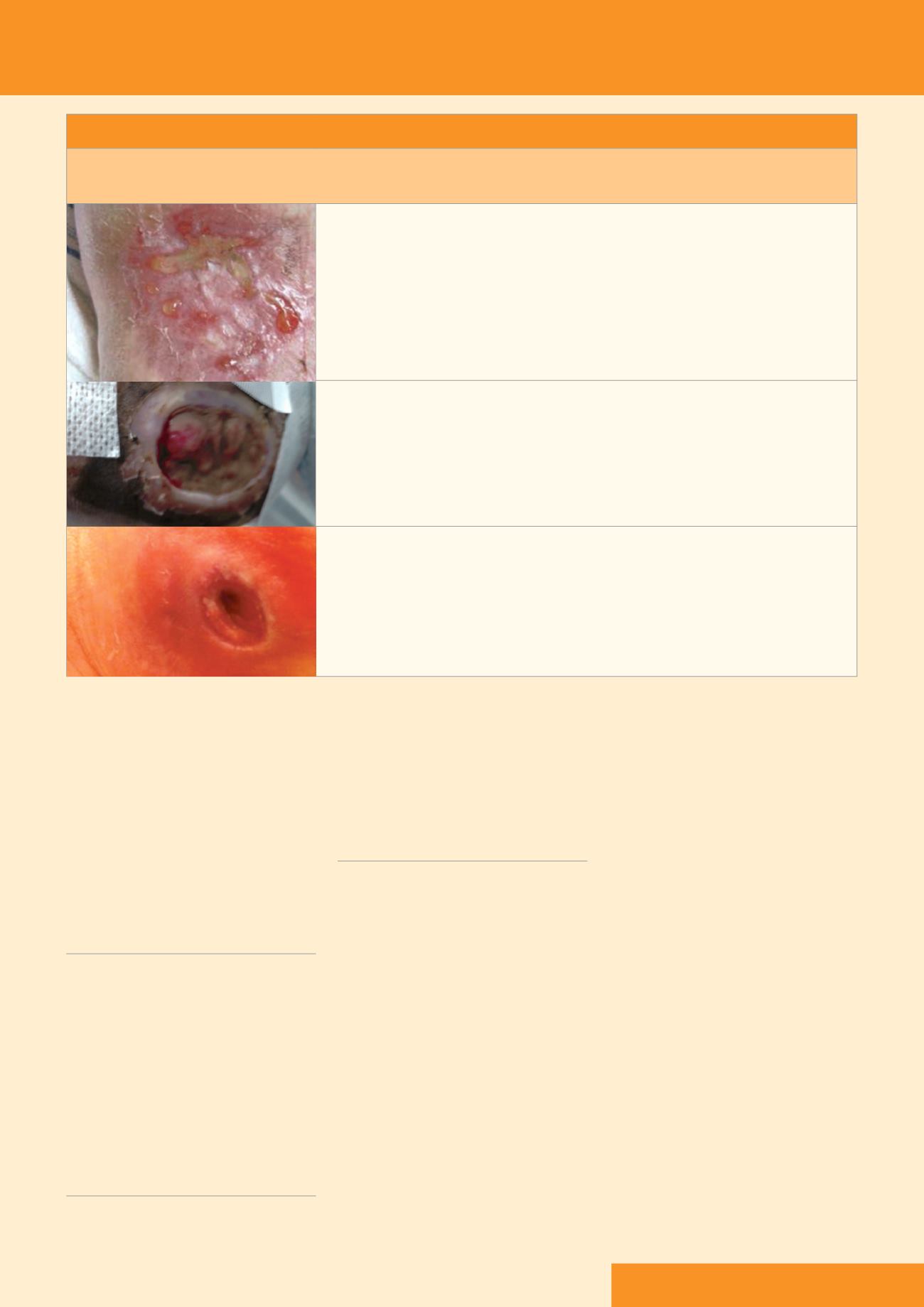
PRESSURE ULCERS
These localised areas of damage to the skin occur as a result of pressure, with
or without shear, usually over bony prominences. Although mainly prevent-
able, the incidence of pressure ulcers still remains high. They have been
identified as ‘never events’ by the Department of Health (DH, 2009), with
prevention being one of the high impact actions (HIAs), and as indicators of
the quality of care being given (Griffiths, 2010).
JCN









