WHAT IS A CHRONIC WOUND?
A wound that has been present for
more than six weeks is generally
regarded as chronic. Acute wounds
heal in a well-organised process,
passing through the normal stages of
wound healing within an expected
time frame for the wound type. For
example, a partial-thickness wound
(i.e. one that extends only through
the epidermis and may involve part of
the dermis, but not the subcutaneous
tissue or underlying structures) is
expected to heal in a week, while a full
thickness wound can take far longer.
Box 1
outlines the normal, overlapping
stages of wound healing. Chronic
wounds do not follow this normal-
healing process but become stuck in
one of the stages, resulting in delayed
healing or a failure to heal.
RISK FACTORS
Healing of a wound may be delayed
by local, systemic or psychosocial
factors (
Box 2
) (Timmons, 2006; Eagle,
2009). The different factors may
interact to promote or delay wound
healing. Any that are identified as
contributing to delayed healing should
be promptly addressed. For example,
improving the patient’s nutrition, or a
change in dressing choice.
HOW DO CHRONIC WOUNDS
DIFFER FROM NORMAL WOUNDS?
Chronic wounds cannot heal
because of cellular and molecular
abnormalities within the wound bed.
Chronic wounds contain elevated
amounts of inflammatory cytokines
and proteases, low mitogenic activity
and cells that respond poorly to
growth factors compared with acute
wounds. Upon healing, this pattern
shifts back to one resembling an
acute healing wound (Ovington
WOUND CHRONICITY
›
Understanding chronic wounds...
4
JCN supplement
2015,Vol 29, No 5
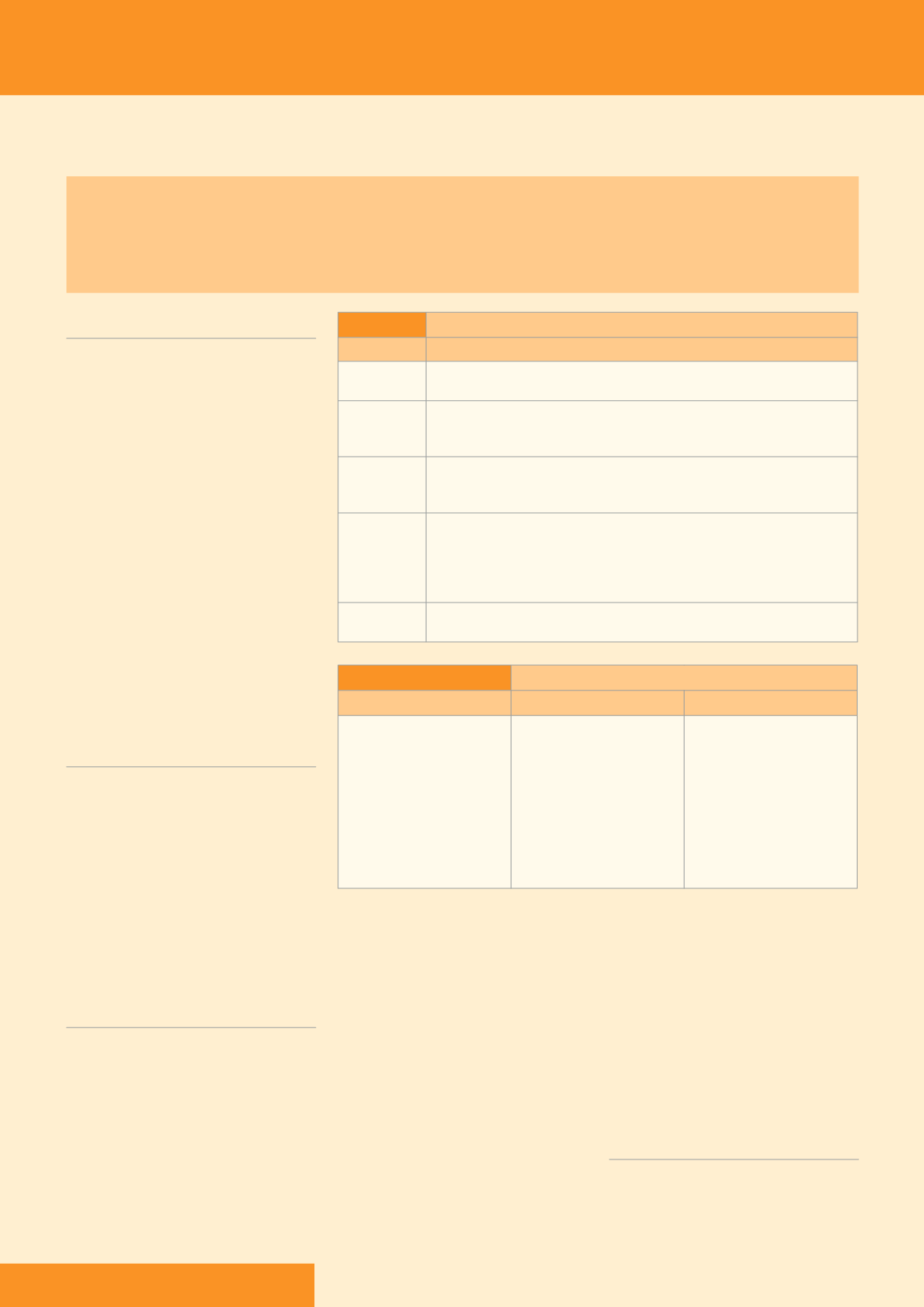
Box 1:
Stages of normal wound healing
Stage
Description
Haemostasis
This is the first stage when the body tries to stop the bleeding if there is a break in
the skin
Inflammation
The preparatory stage of healing, which can last for 0–3 days, as blood vessels shrink to
stop the bleeding (i.e. to use the analogy of a disaster in the home, this stage could be
seen as similar to when the emergency services first arrive [Shipperly and Martin, 2002])
Destruction
This is when the body starts to remove necrotic tissue and any debris from the
wound, which can last for about 2–6 days (i.e. when the refuse collectors arrive
[Shipperly and Martin, 2002])
Proliferation
This is when the body starts to repair the damage (about three days after the injury) and
the wound bed starts to fill up with new, collagen-rich tissue and new cells grow. The
duration of this stage is dependent on the size of the wound but can take up to several
weeks (i.e. the builders arrive and put up their scaffolding in preparation for repairing
the damage [Shipperly and Martin, 2002])
Maturation
This is when epithelial tissue covers and closes the wound (i.e. the final stage when the
decorators arrive [Shipperly and Martin, 2002])
Chronic wounds are increasing in prevalence as the population ages and the number of people living with multiple
comorbidities that put them at risk of developing wounds rises (Gottrup et al, 2013). As the majority of care for chronic
wounds is carried out in the community setting (Posnett et al, 2009), it is important that clinicians understand wound
chronicity, its causes, the consequences for the patient and healthcare provider, and how to identify and manage the
cause of wounding so that chronicity can be avoided where possible.
Box 2:
Risk factors for developing a chronic wound
Local factors
Systemic factors
Psychosocial factors
Local infection
Hypoxia
Trauma
Presence of foreign bodies
Chronic wound exudate
Mechanical stress
Temperature
Comorbidities such as:
›
Diabetes mellitus
›
Malnutrition
›
Immunodeficiency
›
Medication
›
Renal disease
›
Rheumatoid arthritis
›
Age
›
Circulatory insufficiency
Living environment
Lifestyle
and Schultz, 2004). Inflammation is
a hallmark of chronicity, as chronic
wounds often stall in the inflammatory
stage (Werdin et al, 2009). Signs and
symptoms of chronicity include:
Moderate-to-high exudate levels,
the presence of which further delays
healing (Vowden andVowden,
2004). Chronic wound exudate has a
different composition to acute wound
fluid with high levels of inflammatory
mediators and activated matrix
metalloproteinases which have a
negative effect on healing
Oedema in wounds where there
is venous insufficiency. This is
characterised by chronic swelling
caused by excessive fluid in
the tissues
Low perfusion and hypoxia: chronic
wounds often have an inadequate
blood supply which causes delayed
healing and unhealthy formation
of granulation tissue (Younes et al,
2006). Overgranulation can occur
because the wound is in a prolonged
inflammatory state, it is occluded,
there is excessive exudate, or there
is a cellular imbalance (Stephen-
Haynes and Hampton, 2010).
CAN CHRONIC WOUNDS
BE AVOIDED?
With appropriate diagnosis and
management, the majority of chronic
wounds can be healed within 24 weeks
(Posnett and Franks, 2007). In practice,









