HOLISTIC ASSESSMENT
8 JCN supplement
2018,Vol 32, No 4
that the agreed self-care plan, which
should include a good skin care
regimen and exercise (Wounds UK,
2015), is a lifelong commitment to
prevent recurrence. In the author’s
clinical experience, involving and
informing family and carers can also
help to support the patient to take
ownership of their condition.
Guidelines support the continued
use of compression hoisery or wraps
to reduce the risk of recurrence of
ulceration, which should be applied
at the strongest compression that
a patient can tolerate (SIGN, 2010;
Wounds UK, 2016).
Along with prevention therapy,
patients should be reassessed at
regular intervals during the first
year post wound healing. It is
recommended that this takes place
at three, six and 12 months, and
thereafter annually (Wounds UK,
2016). Where clinically indicated,
and in concordance with local policy,
reassessment may need to include
repeat ABPI to check that there have
been no changes in arterial status
and that the patient remains suitable
for compression therapy (Freeman,
2017). Reassessment should,
therefore, also be part of the local leg
ulcer care pathways.
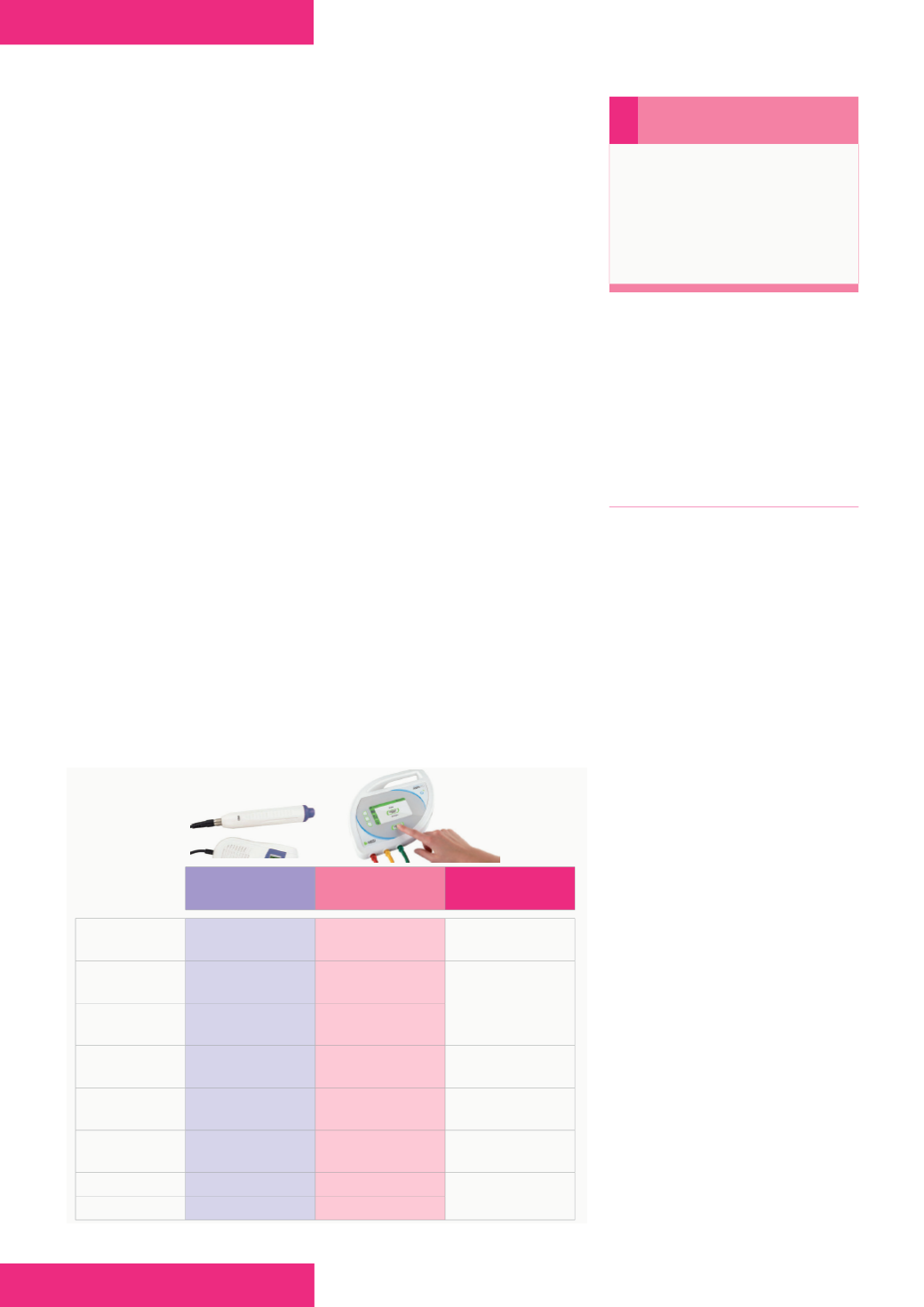
Figure 1.
Use of MESI ABPI MD compared with the doppler probe.
despite wound healing. This provides
an opportunity for clinicians to
review any problems that a patient
may have through holistic-based
discussions, as patients can attend
for review at any time through the
‘well leg’ pathway, rather than just at
pre-agreed intervals.
CONCLUSION
The high prevalence of leg
ulceration in the UK, which results
in the utilisation of significant NHS
resources, presents many challenges
to anyone involved with caring for
patients with lower leg problems.
Ultimately, any assessment should
incorporate a full holistic approach to
provide accurate diagnosis and care
planning at an early stage. Healthcare
professionals have a duty of care to
ensure that they have had training
and have the adequate competencies
to undertake lower limb care.
Along with full holistic history-
taking, vascular assessment is a key
component of lower limb assessment.
However, time pressures in primary
care can impact on a clinician’s ability
to complete an ABPI to exclude
arterial disease. Healthcare providers
need to ensure that staff have
sufficient time allocated and consider
modern technology to assist clinicians
in offering adequate and timely
appointments. The incorporation of
a psychosocial model, such as the
Leg Club
®
, gives an opportunity
for an evidence-based approach to
patient-centred care and to promote
ongoing preventative support.
Overall, early intervention,
improving essential wound
assessments and promoting self-
care can significantly reduce patient
suffering, improve patient outcomes,
and save NHS resources.
JCN
i
Remember
‘Improving the assessment of
wounds’ was specified as a key
goal of the Commissioning for
Quality and Innovation (CQUIN)
scheme for 2017–2019 (NHS
England, 2016).
DOPPLER
PROBE
MESI ABPI MD ABPI MD USE
ARGUMENTS
Measurement
duration
30 minutes
1 minute
Plethysmographic
method
Pre-measurement
resting
10–20 minutes
0 minutes
Elimination of blood
pressure drift error
and time-saving
Measuring
process
One extremity
at a time
Simultaneous
Additional
education
YES
NO
Medical staff are
familiar with the cuffs
Calculations
Manually
Automatic
Instant left and right
ABI and more accuracy
Measurement
report
NO
Automatic via PC
For the patient record
and insurance billing
Clothes removal
YES
NO
Increased patient
comfort
Gel appliance
YES
NO
JCN
To facilitate patient self-care,
healthcare professionals should
develop a therapeutic, non-
judgemental relationship by
listening to any concerns that
they might have, managing their
expectations, and empowering
them to make decisions about the
best options for lifelong prevention.
Any maintenance system should be
simple and practical to use (Wounds
UK, 2015), so that it fits in with a
patient’s lifestyle.
With time being a rare
commodity in the community,
models of care such as Leg Clubs
provide opportunities for patients
to receive ongoing care and advice
to prevent recurrence, along with
the provision of early intervention
should a problem arise, due to their
unique ethos of ‘no appointment
necessary’. The model breaks
traditional boundaries and evidence
demonstrates that patients who
attend Leg Clubs have better
healing and lower recurrence rates
than those treated in conventional
settings (Lindsay, 2017).
Ongoing maintenance, as part
of the ‘well leg’ regimen, is a core
aspect of the Leg Club model,
where a patient’s care never ends