6
JCN supplement
2018,Vol 32, No 4
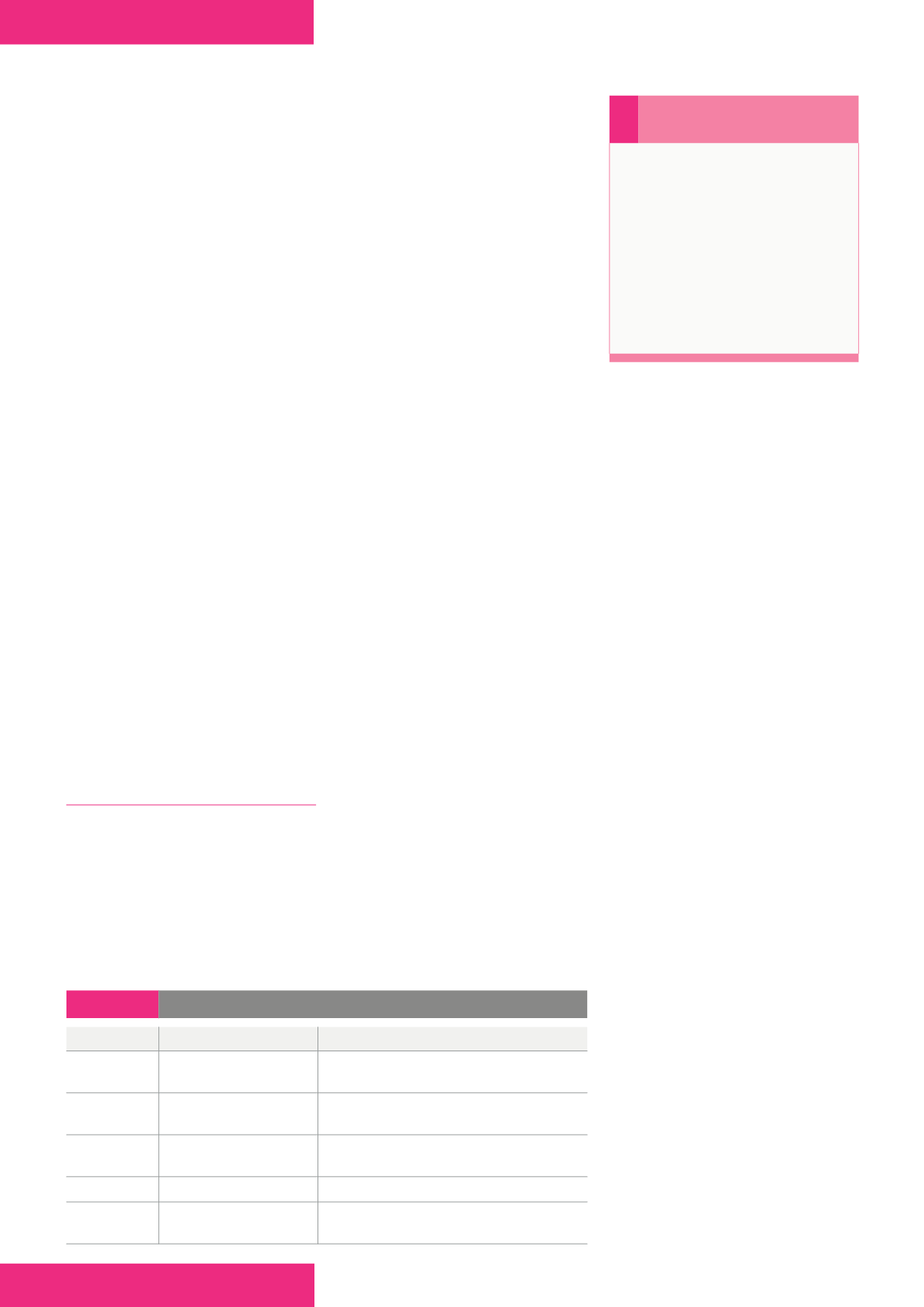
HOLISTIC ASSESSMENT
Although completing an ABPI
reading is not a diagnosis of venous
disease (Wounds UK, 2016), it
assesses for underlying arterial
involvement and so can guide the
level of compression that may be
used (
Table 2
).
The optimum treatment for
venous leg ulcers is recognised as
being 40mmHg compression therapy
graduated from the ankle upwards
(SIGN, 2010). Indeed, best practice
guidance advises that any patient
requiring compression levels greater
than 17mmHg should have a vascular
assessment (Wounds UK, 2016) to
establish the underlying vascular
status before applying compression
therapy. For those wounds caused by
arterial insufficiency, treatment with
compression is contraindicated, as
it could potentially restrict arterial
perfusion causing further harm
(Mosti et al, 2012). Patients with a
mixed aetiology ulcer may benefit
from reduced levels of compression
of between 20 and 30mmHg. Without
diagnosing the underlying aetiology
of a leg ulcer, it is not possible
to provide the correct treatment.
Therefore, full vascular assessment is
vital to establish the correct level of
compression to be applied, or if it
is contraindicated.
CHALLENGES/BARRIERS TO
FULL ASSESSMENT
With demands on healthcare
professionals’ time within the
community, it can be challenging to
dedicate sufficient time to undertake
thorough assessment of patients
with leg ulcers. A key principle in
delivering safe and effective practice
is that healthcare professionals
receive competency-based training;
this is imperative in leg ulcer
management. However, this can
prove challenging in community
and practice nursing, where teams
may be smaller and securing time
out of the work environment can
be difficult. Furthermore, as staff
may work in relative isolation,
it can be challenging to ensure
competency-based assessment
with an adequately trained mentor.
However, Leg Clubs
®
can support
the standardisation of education,
provide an environment for
healthcare professional development
and a teaching resource for
research-based wound management
(Hampton, 2016).
Too often, in the author’s clinical
experience, short appointments
are given to patients requiring
leg ulcer care within busy clinical
settings, leading to limited history-
taking, ineffective assessment, and
subsequently poor care planning.
Adequate time needs to be allocated
for full holistic assessment, as this
will guide the clinician in their
care planning. Furthermore, to
provide holistic care, treatment
pathways need to be undertaken
in partnership with the patient
(Stanton et al, 2016).
Knowledge and training are
paramount for any clinical skill
and this is no different with leg
ulcer care. Healthcare professionals
need to receive regular, up-to-date
training so that they have the current
knowledge and competencies
required to undertake all aspects of
leg care, including full assessment
and management, based on best
practice (Wounds UK, 2016).
Barriers to ABPI assessment
While the importance and relevance
of ABPI assessment is largely
reported, Guest et al (2015; 2018)
highlighted that it is not being
carried out often enough. This
could be because there are potential
barriers to its completion.
First, when should you assess a
patient with a wound to the lower
limb? There is often a gap between
presentation of a patient with a
wound and completion of holistic
assessment, including vascular
examination. It has previously been
recommended that any wound
which has failed to heal within six
weeks be defined as an ulcer and
that a full assessment should be
scheduled (Royal College of Nursing
[RCN], 2006). However, more
recent guidance suggests that a leg
ulcer is defined as a break on the
skin which fails to heal within two
weeks (National Institute for Health
and Care Excellence [NICE], 2016).
Therefore, a full holistic and vascular
assessment is recommended if a
wound fails to heal within this two-
week period, and, ideally, within 10
days from presentation if the patient
has any skin changes or oedema
associated with venous disease to aid
prompt diagnosis of aetiology and
initiation of appropriate treatment
(Wounds UK, 2013).
With the current recommendation
for patients to be treated at the
earliest possible opportunity, it is
suggested that appropriate patients
with acute wounds to the lower limb
(i.e. those with an initial diagnosis,
no signs of critical ischaemia, intact
sensation and a normal limb shape),
›
Remember
Measuring ABPI:
Aids holistic lower
limb assessment
Aids diagnosis of
ulceration aetiology
Guides level of
prescribed compression
Identifies need for further
investigations and/or onward
referral to specialists.
Table 2:
ABPI readings (Harding, 2015)
ABPI reading Indication
Compression level
>1.0–1.3
No indicators of peripheral
vascular disease
Apply high level compression therapy
0.81–1.0
Mild peripheral disease
May have high levels of compression therapy;
monitor ABPI
0.51–0.8
Significant arterial disease
May have reduced compression; refer to specialist
nurse/vascular specialist
<0.5
Severe arterial disease
No compression; urgent referral to vascular specialist
>1.3
Measure toe pressures or refer
to specialist
May have compression therapy; liaise with specialist
nurse/vascular specialist