12 JCN supplement
2018,Vol 32, No 4
WOUND DEBRIDEMENT
weeks of conservative treatment with
autolytic debridement at the general
practice there was no improvement
in the condition of the wound and
so, after discussion with the GP, Mr A
was referred to the local plastics unit
for surgical debridement and to the
community tissue viability service.
Mr A continued to receive a further
six weeks of conventional treatment
of twice weekly dressing changes
with hydrogel to encourage autolytic
debridement, but again with little
progress. He was also prescribed oral
antibiotics by his GP, as the GPN
identified signs of wound infection.
At presentation to the tissue
viability clinic after 10 weeks’
treatment, Mr A’s wound was covered
with necrotic, leathery eschar (
Figure
3
). As no staff were trained to remove
the eschar with sharp debridement,
UCS premoistened debridement
cloths were used to mechanically
debride the wound twice weekly.
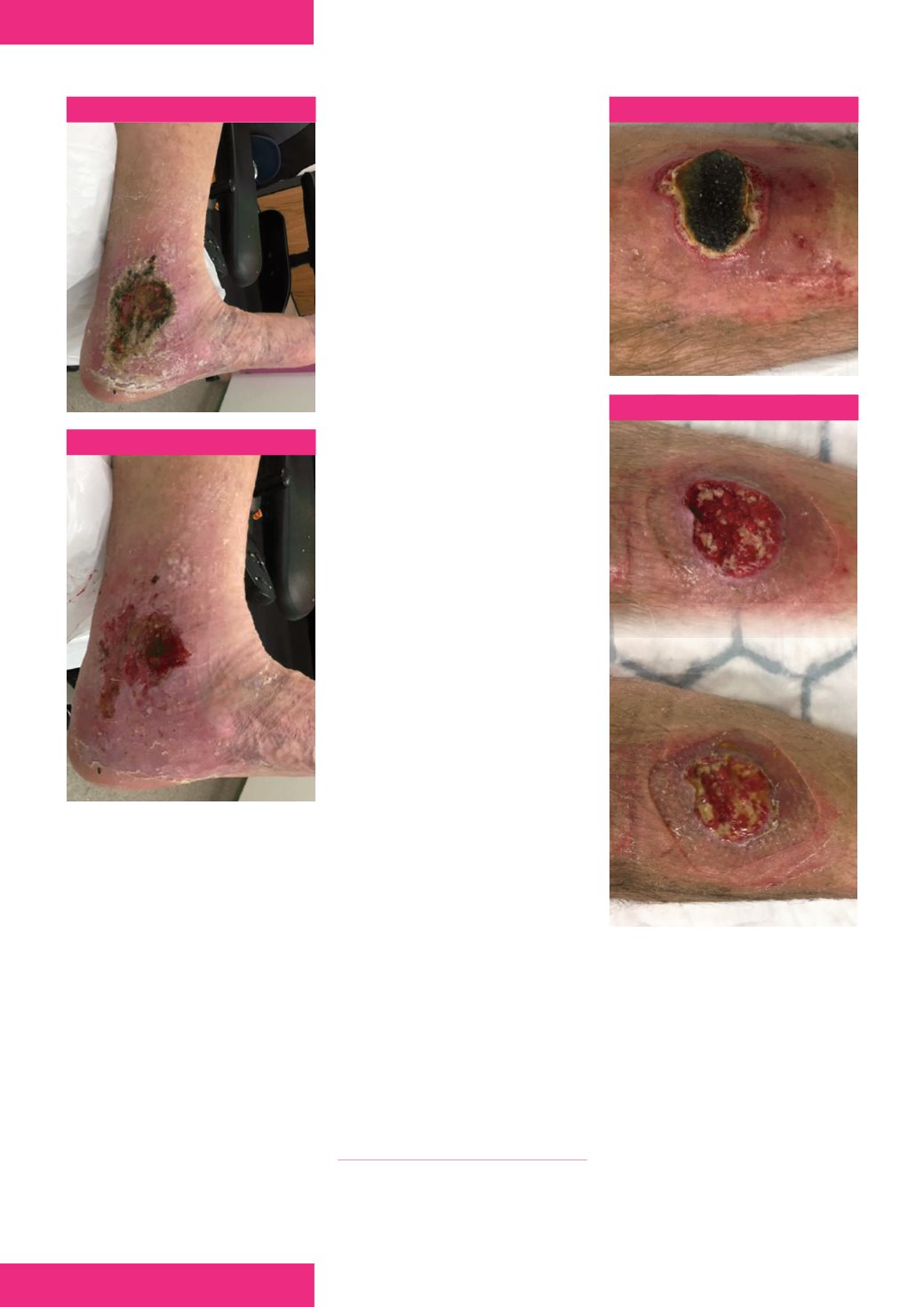
After just one week, the eschar had
lifted leaving islands of granulation
tissue in a sloughy wound bed
(
Figures 4
and
5
).
Mr A’s vascular assessment showed
no signs of arterial insufficiency so
compression therapy was started. As
he was active and wanted to continue
to enjoy playing in his bowls team,
he was anxious and concerned about
compression bandages restricting his
activity. He had little oedema in his
lower limb and so was fitted with a
juxtalite
®
compression wrap device
(medi UK). This also allowed him to
manage his personal hygiene needs
and skin care during treatment. After
two further weeks and four clinic
visits, the condition of the wound
bed had greatly improved — wound
edges had advanced and a reduction
in wound size could be seen. After
three weeks of treatment at the tissue
viability clinic, he was discharged back
to the GPN with a self-care regimen,
involving skin care and compression
therapy with juxtalite, as surgical
referral was no longer required.
BIOFILM MANAGEMENT
A biofilm is a complex microbial
community, consisting of bacteria
embedded in a protective matrix
of sugars and proteins commonly
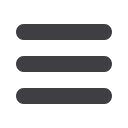
Figure 3.
Figures 4 and 5.
4
5
with the result, as he said that the
ulcers were becoming uncomfortable
under bandages and beginning to
itch, but that he found the process of
debridement soothing.
Case report two
Mr A was an 80-year-old, retired
gentleman, who had a healthy and
active lifestyle. He had no particular
past medical history or comorbidities.
He presented to the tissue viability
clinic for leg ulcer assessment
following referral from a general
practice nurse (GPN) for leg
ulcer management.
During a game of bowls 11 weeks
earlier, he had tripped and obtained a
traumatic pre-tibial laceration to his
left leg. He saw his GPN on the day
of injury and started twice weekly
dressing changes. However, after four
Figure 1.
Figure 2.
found in chronic wounds (Keast
et al, 2014). Recent literature has
demonstrated increasing awareness
of their presence in the majority of
non-healing wounds (Malone et al,
2017), and the role that biofilms play
in delayed wound healing (Metcalf et
al, 2014; Schultz, 2015).
Biofilms provide a protective
environment for microorganisms
embedded within them, improving
their tolerance to the host’s immune
system, topical antimicrobial agents
and environmental stresses, which
is why they can stall wound healing.
It is important to physically remove