JCN supplement
2018,Vol 32, No 2
9
EVIDENCE-BASED PRACTICE
GRADING EVIDENCE
The grading and presentation of
evidence for clinical implementation
has developed in two directions:
An extensive critical appraisal of
all the published and presented
information on a subject, but
which only includes RCTs
with clear definitions, blinding
and randomisation, in any
final study. An example is the
Cochrane systematic review
on compression for venous
leg ulcers (Cullum et al, 2009,
updated from 2001)
An approach that focuses not
only on level 1 evidence, such
as RCTs, but includes all levels
of evidence, for example
guidance from the National
Institute for Health and Care
Excellence (NICE) (Leaper,
2009). An example in wound
care includes the NICE (2008)
study, ‘Surgical site infection:
prevention and treatment of
surgical site infection’.
The second of these approaches
involves interested clinicians and
scientists who analyse the available
evidence. The evidence is still
graded for its level of excellence,
but this approach allows experts
to formulate clinical guidelines,
particularly in the absence of high-
level evidence. In a field such as
wound care where the amount of
level 1 evidence is small, guidelines
supported by expert opinion are
critical to support and improve
wound care practice.
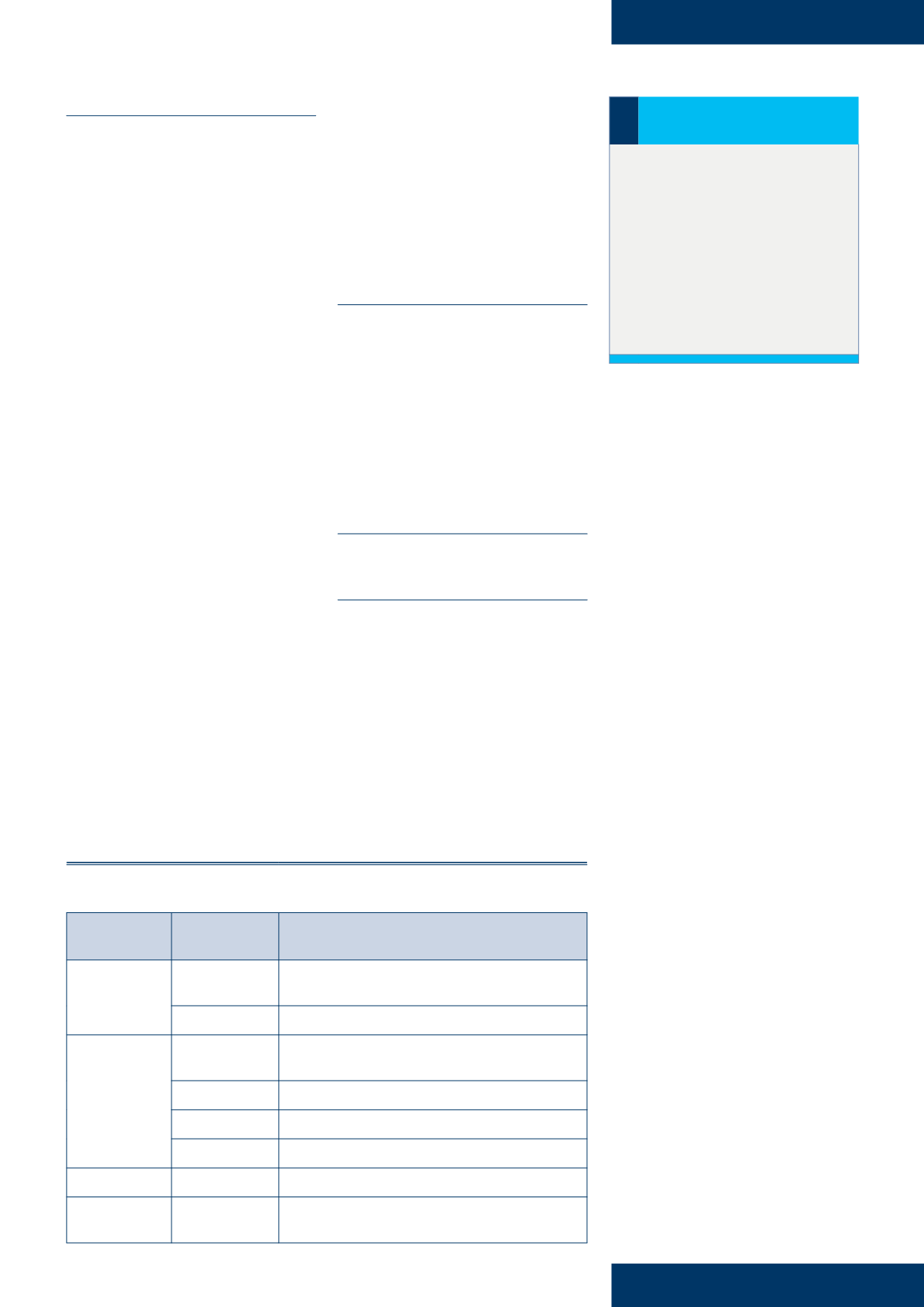
When all levels of evidence have
been included in the review, they
will usually be graded in terms of
recommendations for practice, i.e.
from A–D, with recommendation A
being the highest (
Table 1
).
However, lack of knowledge is
not an excuse for a nurse failing to
provide the patient with the best
possible wound care and, if a nurse
was to be challenged about poor
care, it would not provide a robust
defence. Therefore, nurses treating
wounds need to ensure that their
knowledge and practice are based
on the most up-to-date evidence.
Where barriers exist, they need to be
identified and raised as a concern or
a patient safety issue.
The wound management
literature includes a confusing
array of tools, models, evidence-
based protocols, guidelines and
algorithms, which are all aimed at
improving clinical decision-making
(Flanagan, 2005). However, if these
guidelines are to be practically
applied, they need to appraised,
made simple, and contextualised
for practice. Local tissue viability
specialists and link nurse support
groups can make a valuable
contribution to ensuring evidence-
based practice becomes a reality
and can provide a good source of
knowledge for community nurses.
Dressing manufacturers should
also be able to supply a summary
of available research for individual
products; the nurse can then
draw conclusions about the level
of evidence presented using the
hierarchy of evidence model
(
Table 1
).
There are a number of strategies
that can be used to support the
implementation of research evidence
into practice and effective models
include the five-step process, which
is often referred to as the 5As and is
Table 1:
Study design and level of evidence with grade of recommendation (Oxford Centre for
Evidence-based medicine, 2001)
Grade of
recommendation Level of evidence Type of study
A
1a
Systematic review of (homogeneous) randomised controlled
trials (RCTs)
1B
Individual RCTs (with narrow confidence intervals)
B
2a
Systematic review of (homogeneous) cohort studies of
‘exposed’and‘unexposed’subjects
2b
Individual cohort study/low-quality RCTs
3a
Systematic review of (homogeneous) case control studies
3b
Individual case control studies
C
4
Case series, low-quality cohort or case control studies
D
5
Expert opinion based on non-systematic reviews of results or
mechanistic studies
‘Evidence is of little benefit
to the patient unless it is
implemented in practice.
There are many challenges
in the application of
evidence to practice,
including lack of knowledge,
insufficient time to research
the knowledge, and
organisational barriers...’
BARRIERS TO IMPLEMENTING
EVIDENCE IN PRACTICE
Evidence is of little benefit to the
patient unless it is implemented in
practice. There are many challenges
in the application of evidence to
practice, including:
Lack of knowledge
Insufficient time to research the
knowledge
Organisational barriers, such
as management support for
changing practice (see
practice
point box
).
›
Remember
In wound care, the amount of
level 1 evidence is small due to the
difficulty in comparisons as a result
of the number of patient variables
involved, such as underlying
comorbidities, wound aetiologies,
many of which require treatments
of the underlying condition, e.g.
offloading in patients with diabetic
foot ulceration.