EVIDENCE-BASED PRACTICE
10 JCN supplement
2018,Vol 32, No 2
i
Practice point
Barriers to implementing evidence-
based practice, include:
`
Lack of perceived value for
research in practice
`
Lack of knowledge
`
Insufficient time to
conduct research
`
Difficulty in changing practice
`
Too busy to appraise
the evidence
`
Lack of knowledgeable mentors
`
Lack of education about the
research process
`
Complexity of research reports.
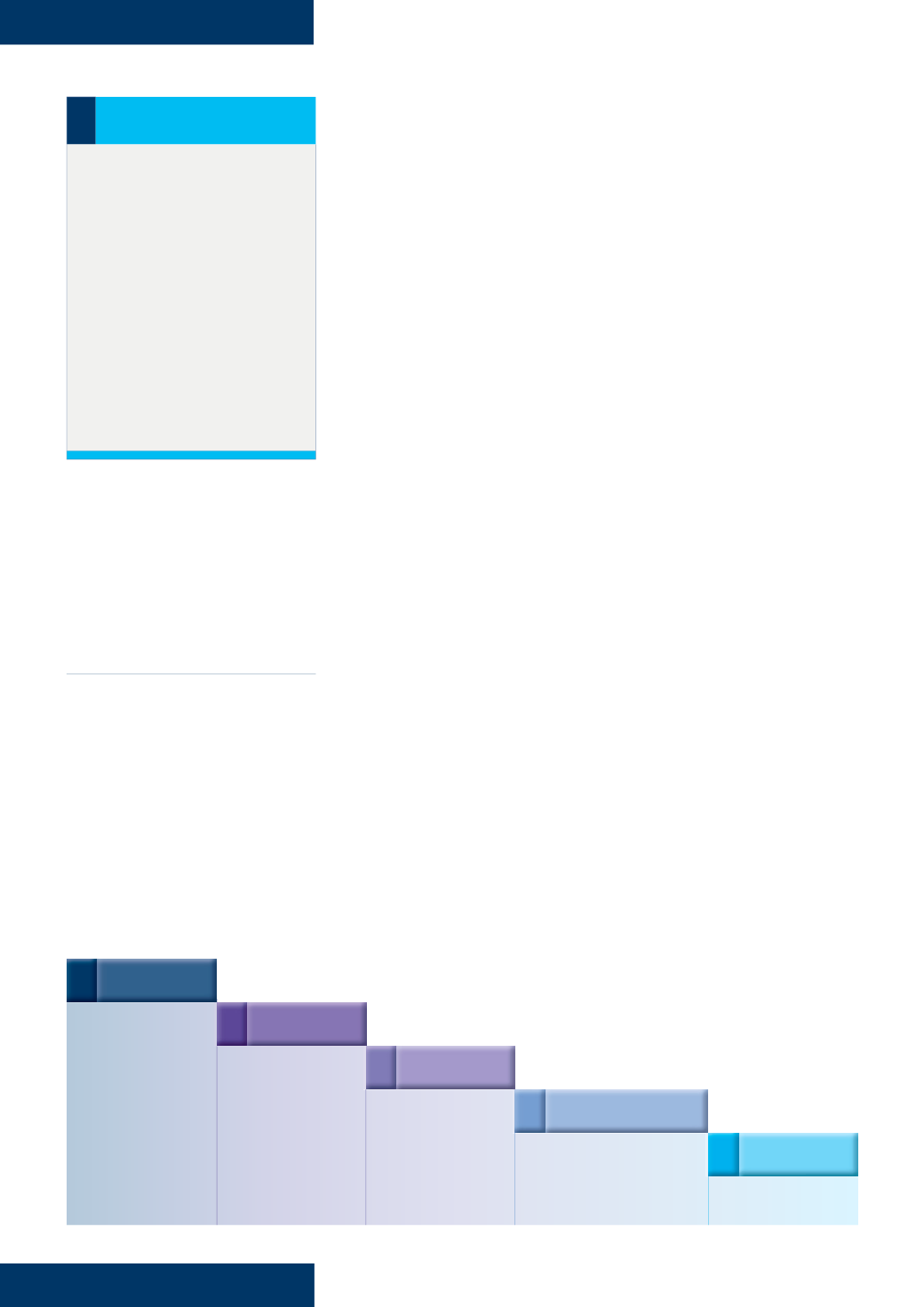
simple and easy to use (Sackett et
al, 2000;
Figure 3
). This model can be
particularly useful for wound care
nurses who are developing wound
care formularies and need to gather
and appraise the evidence to
support the use of a particular
dressing product.
APPLICATION TO PRACTICE
The process of implementing
evidence-based practice primarily
focuses on assessing whether an
intervention will solve a clinical
issue, or posing a question such
as,‘What is the best wound care
treatment to heal the patient’s
wound?’. The nurse then has
to access the relevant data and
evidence available from a variety
of sources. However, the reality
in clinical practice is that nurses
are faced with difficult treatment
choices, including a vast array of
products, and want to achieve the
best outcomes for their patients.
As mentioned above, wound care
companies can often provide an
evidence-based summary for their
products and several best practice
and consensus documents can be
accessed freely online, for example
the European Wound Management
Association (EWMA) position
document on hard-to-heal wounds
and the World Union of Wound
Healing Societies (WUWHS)
consensus document on surgical
wound dehiscence (EWMA, 2008;
WUWHS, 2018).
There is often a paucity of
evidence presented for a wound
care intervention and the nurse may
have to identify the best way forward
through critical appraisal of the
evidence that does exist to decide
whether it is methodologically
appropriate, rigorous and clinically
relevant. Findings need to be
applied to practice and the
effectiveness of the intervention
evaluated through reassessment.
There are many variables that
will influence wound healing, for
example, blood glucose control
in patients with diabetic foot
ulceration, and the nurse needs to
take these into consideration as
well as selecting an evidence-based
wound dressing. It is also necessary
to balance the recommendations
contained in systematic reviews,
RCTs and observational studies, with
clinical expertise and feedback from
colleagues and patients, all of which
will support the nurse to make best
practice decisions (Dowsett, 2017).
When making treatment decisions
for patients, it is important to:
`
Address the underlying cause of
the wound
`
Treat underlying comorbidities
`
Optimise the wound bed
through debridement, exudate
management, and infection
prevention and control
`
Provide the most appropriate,
evidence-based treatment.
Ongoing reassessment
and wound measurement will
provide useful information on the
effectiveness of the intervention, and
measuring outcomes such as healing
rates is critical to demonstrate the
success of treatment.
Applying evidence to practice
in wound care can result in
reduced healing time, prevention
of complications and reduced
healthcare costs (Dowsett, 2015).
Advances in wound care and new
treatment options offer clinicians an
opportunity to change the wound
environment and improve healing.
Looking at treatments which can
effectively reduce healing time,
clinicians should be aware of the
clinical evidence for such products
and be able to make an informed
choice about their selection for
treating patients. There is evidence
that dressings directed at inhibiting
matrix metalloproteinases (MMPs)
can reduce healing time in a variety
of wounds, and therefore improve
patient outcomes.
A number of studies have
demonstrated their efficacy in
improving healing rates in leg ulcers,
diabetic foot ulcers and pressure
ulcers (Schmutz et al, 2008; Meaume
et al, 2012; 2017). Diabetic foot
ulcers are a particular challenge
for patients and community
practitioners and evidence to
support any particular treatment
has been poor. However, a recent
randomised double-blind clinical
Figure 3.
The five-step evidence-based practice process.
1 ASK
Formulate an answerable
clinical question
5 ASSESS
Evaluate the effectiveness
of the process
2 ACCESS
Track down the
best evidence
3 APPRAISE
Appraise the evidence for
its validity and usefulness
4 APPLY
Integrate the results with your
clinical expertise and your patient
values/local conditions