8 JCN
2015
JCN Roadshow
T
his session examined the
benefits of debridement and
how it can help nurses to
better view the wound bed, thereby
increasing the chances of accurate
assessment and, in turn, appropriate
treatment.
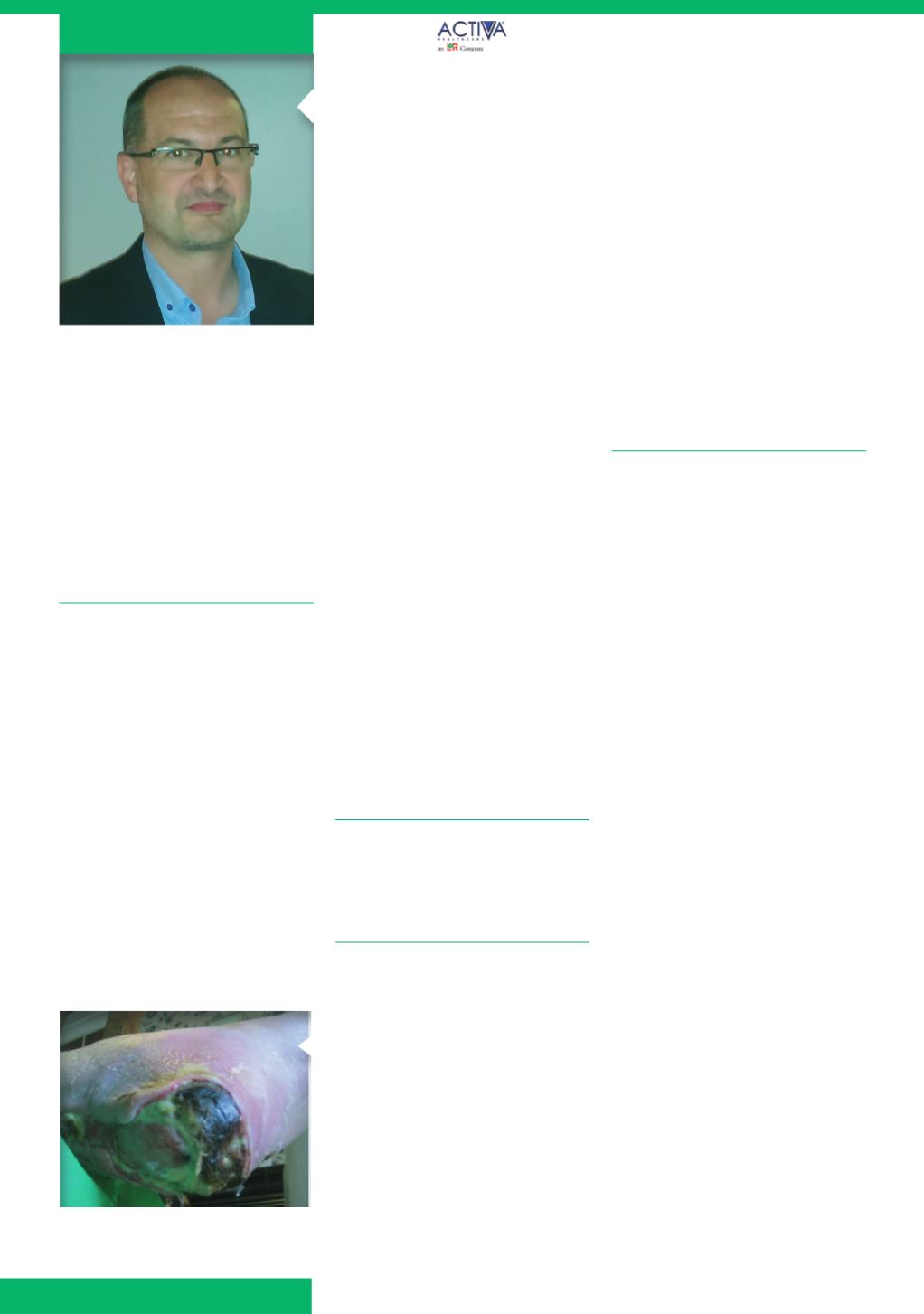
WHAT IS DEBRIDEMENT?
The session began by offering
the audience a definition of
debridement, namely that it involves
the removal of devitalised tissue
from the wound and surrounding
skin (
Figure 1
). This includes removal
of hyperkeratosis and devitalised
tissue and as such debridement
forms part of the wound bed
preparation process.
Like any other element of
treatment, it is important that nurses
who practise debridement are aware
of the variations in method, as well
as the limitations of their own skill
and competency.
Debridement is considered to be
a beneficial component of wound
GETTING STARTED
The session went on to outline
that debridement should not just
be the realm of the specialist — it
is a technique that can be used by
all clinicians providing they have
attained an appropriate level of
competency.
It is also important that the
method of debridement selected
meets the needs of the patient and
is not limited by the nurse’s skills
(Gray et al, 2011), for example, if
a patient really requires surgical
debridement but the nurse is not
qualified to provide this, he or she
should consider referral to the
local specialist team, rather than
persevering with a ‘softer’ form of
debridement that may not benefit
the patient long-term.
The session also highlighted that
before debridement is considered,
nurses should bear the following
points in mind:
What is the aim of debridement,
i.e. to promote healing or provide
symptom control?
How quickly is debridement
required and which method will
best achieve this? For instance,
autolytic debridement with
dressings will take a lot longer
than sharp debridement, but may
involve less trauma
How best to debride, e.g. is
there hard, necrotic tissue that
requires surgical intervention,
or could a gentler method such
as softening with a hydrogel
dressing be considered first?
‘As with any other treatment,
it is important that the
nurse has carried out a
structured assessment before
debridement is performed.’
management because (National
Institute for Health and Care
excellence [NICE], 2014):
Devitalised tissue within the
wound may mask or mimic signs
of infection and act as a physical
barrier to healing
Debridement helps to remove
wound debris, sloughy tissue
and exudate, making it easier
to see the condition of the
wound bed.
Devitalised tissue
Devitalised tissue can be caused by:
Infection (seen as inflammation)
Toxins (seen as inflammation)
Trauma/injury
Reduced blood flow, resulting in
death of tissue.
It is important that clinicians
aim to remove devitalised tissue as
quickly and efficiently as possible,
when it is safe to do so and after
an holistic assessment. Wound
debridement should be an integral
element of good wound care,
as outlined in the best practice
statement,
Optimising Wound Care
(Wounds UK, 2008).
However, as with any other
treatment it is important that nurses
carry out a structured assessment
before debridement is performed
(
Figure 2
).
Figure 1.
A heel wound showing
significant devitalised tissue.
Sponsored by
Simon Barrett, tissue viability
nurse consultant
Debridement as part
of the wound
assessment process