(antimicrobial dressing), or
provide protection for the wound
bed (film dressing)? All of these
considerations, and many more,
may influence dressing choice
Professional accountability/the
law: does the nurse have the
correct knowledge and experience
to make an informed decision?
Remember, it is always a good
idea to consult with a colleague if
unsure
Wound classification: is the
wound a pressure ulcer or a
venous leg ulcer? Is it highly
exuding or infected? Arriving
at the correct wound
classification will help with
accurate dressing choice
Cost: one of consequences of
the explosion in wound care
technology has been the range of
products now available. Nurses
may be limited by their local
formulary, but it is important to
bear in mind the cost of different
dressings
The law: nurses are responsible
for their own practice and any
decisions made. Nurses must
ensure that they are acting within
their knowledge base and that they
document all treatment decisions
or changes in wound status.
STIMULATING HEALING
It is important to identify any factors
that are preventing patients from
healing themselves. This can be done
by exploring the ‘pathway’ of their
condition and treatment to date
and identifying factors that may be
blocking the healing process.
Nurses should aim to stimulate
healing from the point of injury,
with dressings that can address the
presentation of the wound and are
specifically designed to create the
optimum conditions for healing from
first application.
Finding the right evidence
How does the nurse know when he
or she has chosen the right dressing
for the right patient? Randomised
controlled trials (RCTs) are the best
source of evidence, however, there
are few of these available in tissue
viability, partly due to the difficulty of
achieving consistent sample groups.
Alternatively, case studies can
also provide evidence. Good case
studies should consider all variables
affecting healing and provide visible
evidence of the experience of a
patient with a wound.
Case studies
Some clinical case studies from
the author’s practice illustrate the
points made above about providing
the best environment possible to
encourage wound healing (see case
study boxes).
CONCLUSION
As seen in the presentation above,
no matter what the presenting
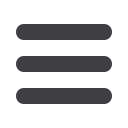
Case 2
This case featured a 47-year-old
man who presented with a leg
injury sustained in a road traffic
accident. This left him with a
lower leg fracture that had healed
following the application of an
external fixator.
However, the patient developed
a chronic leg ulcer, even though
osteomyelitis was ruled out twice
and there was no venous or arterial
disease (this was confirmed by
Duplex scanning).
The patient experienced
repeated infections, which were
treated with manuka honey,
before finally being diagnosed
with leukocytoplastic vasculitis
(a disorder of the skin caused
by small-vessel vasculitis, or
inflammation in the blood vessels).
A management plan was
drawn up with the patient in an
attempt to heal the wound. This
involved a multidisciplinary team
approach, including input from the
dermatology team, a haematologist,
the tissue viability specialist, and
the orthopaedic team.
A biopsy was performed to
determine the cause of new areas
of necrosis and the vasculitis was
treated with steroids.
The new areas of necrosis
were possibly due to an increase
in bacterial burden, therefore the
team decided to use Urgotul SSD
®
(Urgo Medical), for its antibacterial
action, long wear time and ability
to stimulate fibroblast activity in the
wound bed.
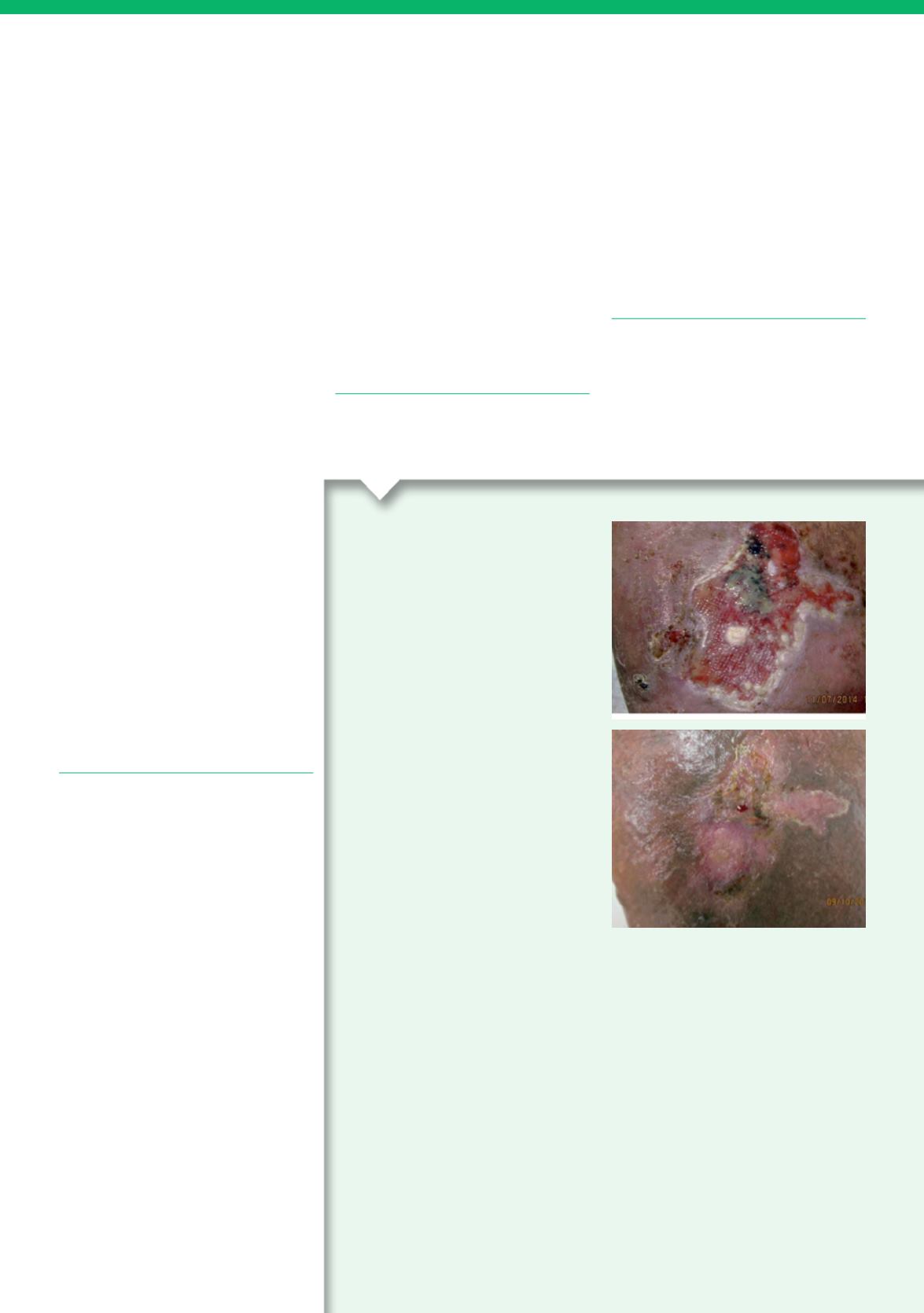
Despite the fact that this wound
was chronic, it went on to heal
completely within three months of
starting treatment with Urgo SSD.
The patient was able to manage
the wound independently and was
pleased with the action of the
dressing and healing outcome.
symptoms and underlying factors
involved in the presentation of
a wound, holistic assessment,
evidence-based dressing selection
and optimising the action of
fibroblasts to stimulate healing can
result in better outcomes for
patients and more cost-effective
wound care.
REFERENCES
Asmussen PD, Sollner B (1993) Mechanism
of wound Healing. In:
Wound Care.
Tutorial Medical Series
. Hippokrates,
Stuttgart
Calvin, M. (1998) Cutaneous wound repair.
Wounds
10(1):
12–32
JCN