COMMUNITY WOUND CARE
JCN supplement
2015 Vol 29 No 5
7
An example of a typical
intervention is ensuring that
patients are nursed on supports
surfaces that are appropriate for
their needs — here the ‘S’ of the
SSKIN bundle should act as a
prompt for nurses to ensure that
the patient is ‘stepped-down’ from
an active mattress to a static foam
mattress for instance.
Similarly, the ‘K’ for ‘keep
moving’ is there to remind nurses
that patients may require help
with changing their position, and
the frequency of this should be
decided by the trained member of
staff on each shift. For instance, a
patient may require fewer changes
of position during the day if they
are undergoing physiotherapy or
occupational therapy. This care
bundle serves to ensure that key
areas of care are covered to aid
prevention in those patients who
are at increased risk of developing
pressure damage.
James et al (2010) reported a
pressure ulcer prevalence of 26.7%
across community hospitals in
Wales — following introduction
of the SSKIN bundle the rates
subsequently fell (Keen and
Fletcher, 2013).
However, in those patients
who have already developed tissue
damage, pressure ulcers can give
rise to significant healing challenges
for clinicians. Category two, three
and four pressure ulcers all require
extensive dressings due to loss of
tissue, along with offloading —
where the area is ‘floated’ using
pillows or by supporting the leg
with devices usually supplied via
occupational therapy — as well as
regular changes in position.
Supplementary dietary intake
may also be required for those
patients whose nutritional needs
have been compromised.
Dressings can range from a
simple hydrocolloid that might
be used to cover a category two
pressure ulcer (Fletcher et al, 2011),
to the use of an alginate dressing
covered with a secondary covering in
a category four ulcer.
foot ulcers and, to a lesser extent, leg
ulcers. The edges of cavity wounds
must be protected, and dressings
used to assist healing from the
base of the wound upwards. This
ensures that there is no ‘undermining’
around the wound edges and that
the optimum tensile strength of the
wound is achieved.
Cavity wounds can be managed
effectively within a community
hospital setting, either with the
more traditional approach of lightly
packing the wound space or by using
topical negative pressure (TNP).
Dressing choice should be
discussed with the patient and
their individual health status taken
into account. By following a logical
pathway an updated plan of care
can be achieved, which should
enhance the patient’s ability to
move through to wound healing
(Harding et al, 2007) (
Figure 2
).
PRESSURE DAMAGE
Pressure damage is known to be
painful and distressing for patients
as well as costly for the NHS, both in
terms of occupied bed days and also
in compensation payouts resulting
from litigation (Bennett et al, 2004).
The introduction of SSKIN
bundles within community hospitals
demonstrated how planned
interventions can make a significant
difference to patients and the care
they receive. SSKIN is the acronym
for
`
6
upport surface
`
6
kin inspection
`
.
eep moving
`
,
ncontinence
`
1
utrition.
Adherence to local wound care
formularies and working with tissue
viability specialist nurses is crucial
when trying to decide on the most
appropriate product.
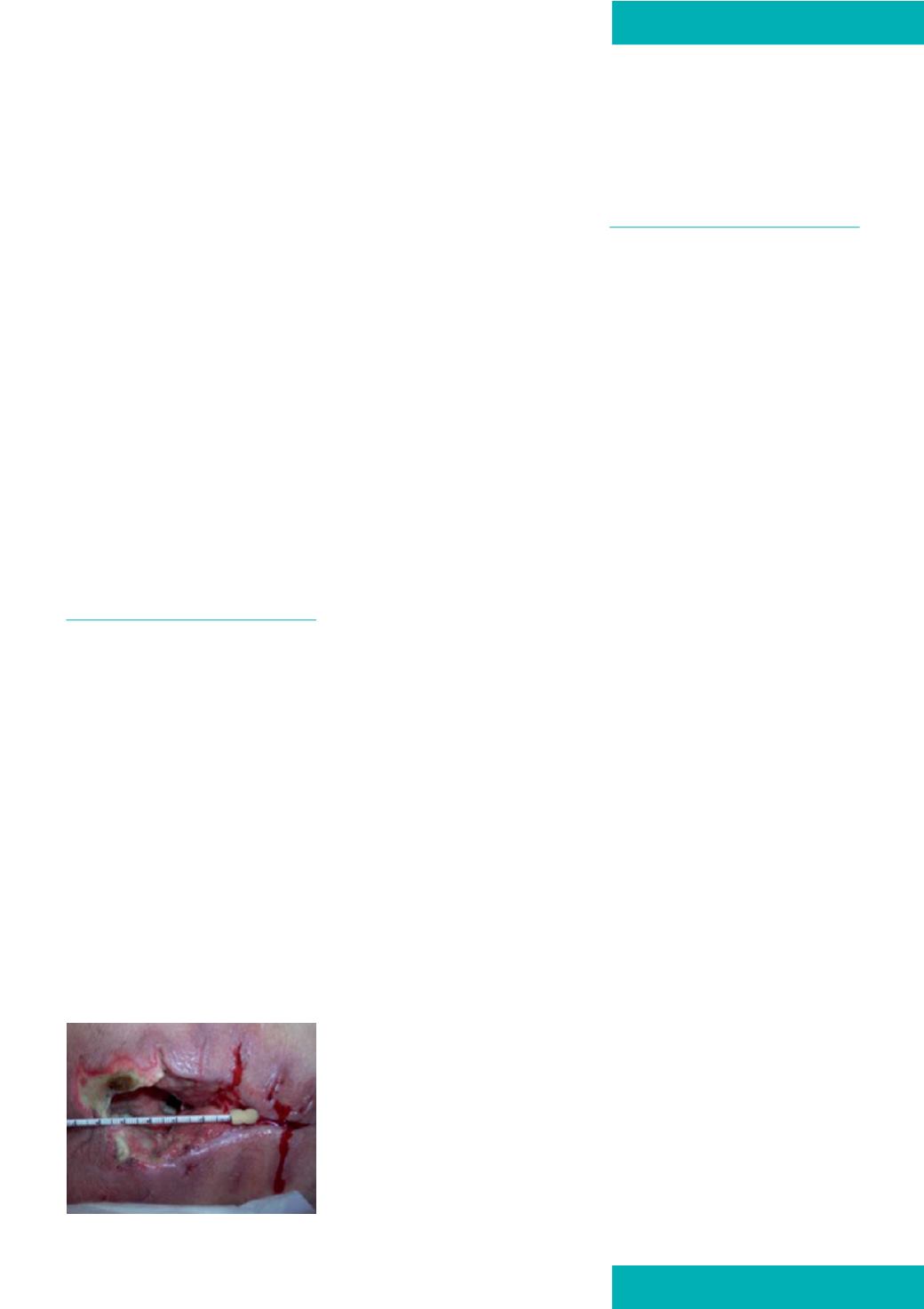
INFECTED SURGICAL WOUNDS
Surgical site infection (SSI) occurs
within a wound following either
keyhole or open surgery (National
Institute for Health and Care
Excellence [NICE] 2008), and is
usually identified by localised pain
at the wound site, heat, pyrexia and
tachycardia (Cutting and White,
2005). SSI rates are closely monitored
by infection prevention teams.
The first line of treatment in SSI
is a course of antibiotics, however
in severe cases the original surgical
incision site may dehisce — this
is where the wound itself has
insufficient strength to withstand the
forces placed upon it and the edges
come apart (
Figure 3
) (Bale and Jones,
2006). This can happen at any time,
but usually takes place between 6–10
days postoperatively and requires
further surgical intervention, which
may include debridement and
reclosure or localised debridement
with the wound then being left open
to close by secondary intention.
This kind of intensive long-term
treatment may not be appropriate in
the patient’s home and, particularly
bearing in mind the increased
cost of extra days spent in hospital
(Coello et al, 2005), the community
hospital could offer a safe and cost-
effective alternative.
Many wounds that have
dehisced due to infection present
with a cavity, which needs to heal
by primary intention from the
base upwards. Once they have
been packed and redressed daily,
many dehisced wounds are then
treated with TNP, which is able
to manage the large volume of
exudate associated with wound
infection. TNP also facilitates rapid
wound closure, as well as improving
patients’ quality of life by reducing
the number of dressing changes.
Although in the past TNP was
regarded as too expensive and only
Figure 3.
A typical dehisced wound.









