50
WOUND CARE TODAY
2017,Vol 4, No 1
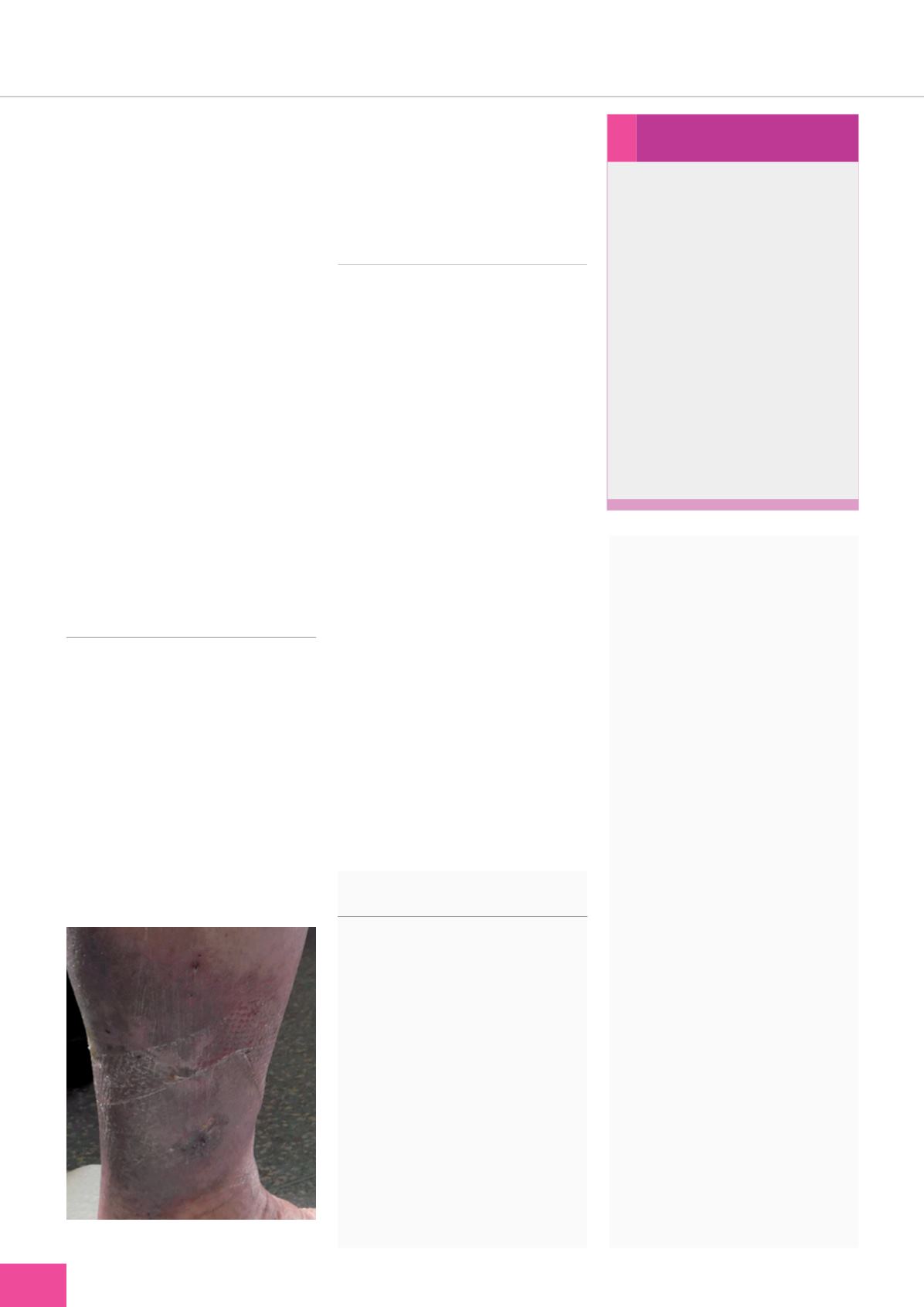
›
go away on holiday without the risk
of his leg deteriorating as a result of
being unable to have his bandaging
applied. On his return, he continued
to wear the hosiery kit and one
month later the ulcer had healed
(
Figure 3
). He stated:
Being able to wear a hosiery kit
rather than bandages made me
feel so much more human; more
normal and civilised. The kit
also felt more comfortable than
the compression bandages and I
could again do things that I once
took for granted, like showering
and wearing normal shoes.
As well as healing the ulcer, I
feel that wearing the hosiery kit
has helped me to understand
the rationale behind wearing
compression hosiery and, in
some way, has given me a
greater confidence in what
hosiery can achieve.
PREVENTION OF RECURRENCE
Ian continued to wear a hosiery
kit on each leg to prevent DVT
and ulcer breakdown. The use of
hosiery kits both for first-line and
maintenance therapy has been found
to improve concordance (Ashby et al,
2014), as they are more comfortable
than bandaging, more cosmetically
appealing and encourage self-
care — all of which lead to greater
patient empowerment (Tickle, 2015).
Self-care has been found to
reduce recurrence rates (Guest et al,
2015) and, as well as compression
therapy, patients should be
encouraged to maintain a good skin
care regimen, to mobilise as much as
possible (Harding et al, 2015), and eat
a healthy diet (Wounds UK, 2016).
CONCLUSIONS
By carrying out holistic assessment,
the reasons for delayed wound
healing and subsequent wound
deterioration were identified and
a treatment plan put in place
that managed underlying causes,
including venous disease and
infection. Local wound management
focused upon resolving problems
identified during wound assessment.
General assessment and speaking to
the patient identified his reluctance
to undergo compression bandaging,
but that he was able to tolerate it
in the short-term. Once some of
the symptoms of his infection and
underlying venous disease had
resolved, the wound progressed
towards healing, which enabled a
decision to be taken with Ian to use
a compression hosiery kit. This was
conducive to self care, aiding
patient concordance with
compression therapy.
The case presented in this paper was
originally published in the
Journal of
Community Nursing
— Hutchinson K
(2015) What is the patient experience of
healing in a hosiery kit?
J Community
Nurs
29(5):
64–5
REFERENCES
Ashby RL, Gabe R, Ali S, et al (2014)
Clinical and cost-effectiveness
of compression hosiery versus
compression bandages in treatment
of venous leg ulcers (Venous leg Ulcer
Study IV,VENUS IV): a randomised
controlled trial. Lancet 383(9920):
871–9
Chamanga E (2017) Wound bed
preparation: employing the TIME
acronym.
Nurse Prescrib.
Available
online:
www.independentnurse.co.uk/clinical-article/wound-bed-
preparation-employing-the-time-
acronym/153938/
Dowsett C, Newton H (2005) Wound
bed preparation: TIME in practice.
Wounds UK
1(3):
58–70
Franks P, Barker J (2016) Management
of patients with venous leg ulcers:
challenges and current best practice.
Eur Wound Management Association
16(1):
81–7
Guest J, Ayoub N, McIlwraith T, et al
(2015) Health economic burden that
wounds impose on the National Health
Service.
BMJ Open
5(12)
. Available
online:
http://bmjopen.bmj.com/content/5/12/e009283
Harding K, Dowsett C, Fias L, et
al (2015) Simplifying venous leg
ulcer management. Consensus
recommendations.
Wounds
International
. Available online:
www. woundsinternational.com/consensus- documents/view/simplifying-venous- leg-ulcer-managementSimon D (2015) How to improve the
community care of patients with leg
ulcers.
J Community Nurs
29(6):
24–8
Stephen-Haynes J (2007) Leg ulceration
and wound bed preparation: Towards
a more holistic framework.
World
Wide Wounds
. Available online:
www. worldwidewounds.com/2007/october/Jackie-Stephen-Haynes/test.html
Tickle J (2015) How can I improve leg
ulcer care when faced with increasing
service demands?
J Community Nurs
29(1):
20–1
Wounds UK (2016)
Best Practice Statement:
Holistic management of venous leg
ulceration
. Wounds UK, London
›
Self-care...
The promotion of self-care for
patients with venous leg ulcers
can have a number of benefits,
including:
›
Greater involvement in
treatment decisions
›
Improved understanding of
disease process
›
Empowering: ‘I can
help myself’
›
Improved outlook and
improved outcomes
›
Reduced dependence
›
Less time spent travelling
to clinics
›
Less travelling for district and
community nurses.
Figure 3.
Ian’s healed venous leg ulcer.
FOCUS ON
TIMES
WCT