WOUND CARE TODAY
2017,Vol 4, No 1
49
FOCUS ON
TIMES
i
MANAGEMENT
DVT is an identified risk factor for the
development of venous disease and,
in Ian’s case, this had happened. His
failing venous system had resulted
in skin breakdown, oedema and
hyperkeratosis, all of which could be
managed using compression therapy.
However, despite the application
of compression bandaging, the
wound had deteriorated, indicating
a possible problem with wound and
skin infection. Referral was made to a
dermatologist who prescribed a
course of prophylactic antibiotics,
which were to be taken over a
four-month period. The wound
began to improve and the oedema
reduced, aided by the combination of
bandaging and antibiotics.
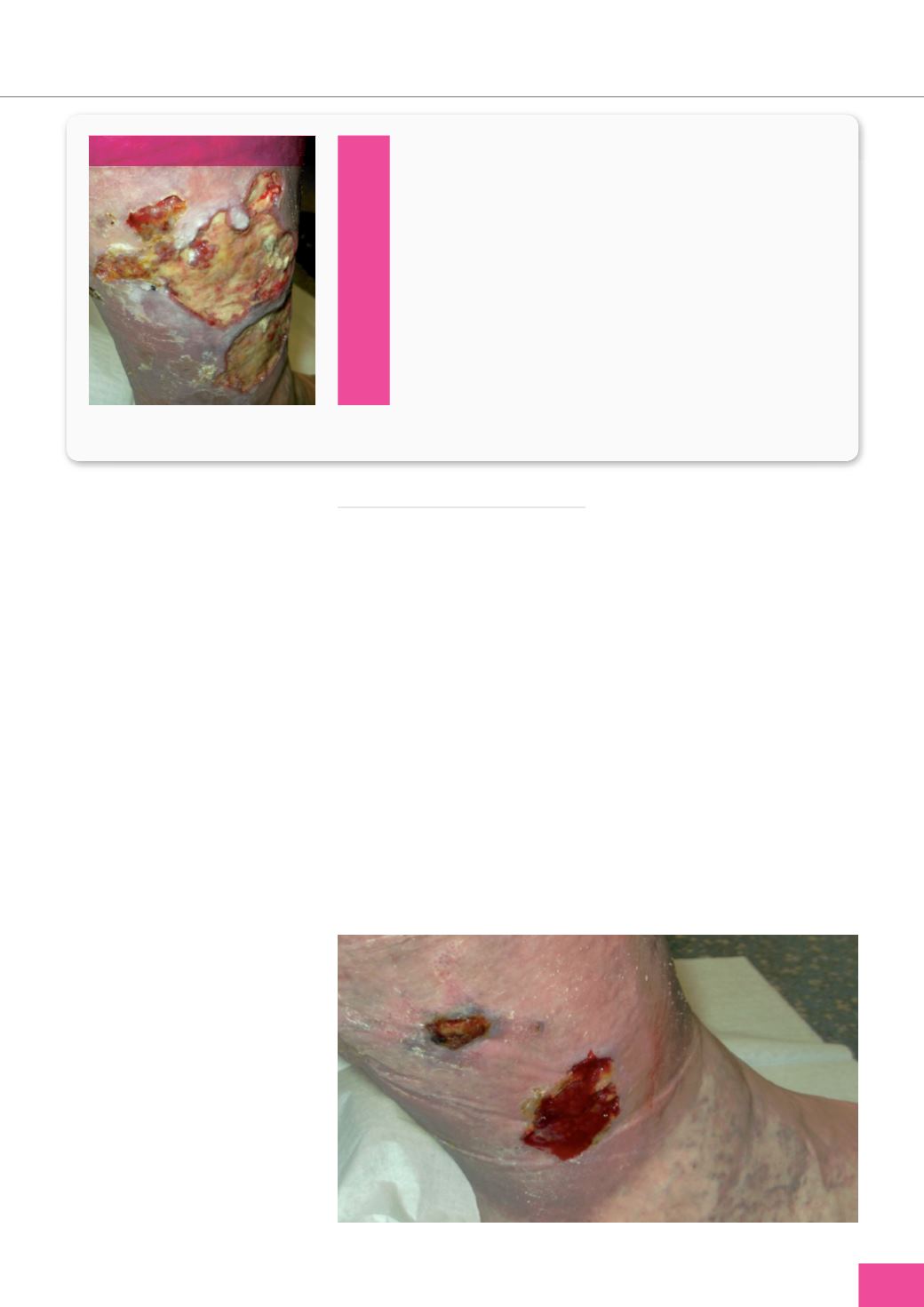
By May 2015, Ian’s ulcer had
significantly improved and reduced in
size (
Figure 2).
The oedema, exudate
volume and pain had all reduced. He
and his wife were planning a holiday,
but he was concerned about how
his compression bandaging could be
reapplied safely and effectively
while away.
A hosiery kit was recommended
following discussion with Ian.
According to Ashby et al (2014),
compression hosiery kits can be
used as a first-line approach forVLU
management and may aid patient
self-care.
As Ian’s limb was oedematous,
ActiLymph
TM
(L&R) hosiery kit
was prescribed.
Ian reported feeling relieved
when trying the kit on that he could
severe oedema and skin breakdown.
Following discharge from hospital,
the ulcer was managed by the local
general practice nurse using wound
dressings and analgesia.
After three months the wound
was deteriorating and the limb
remained oedematous, so referral to
the local leg ulcer specialist service
was made and compression therapy
started. The ulcer was producing
a large volume of exudate and
dressings were required so bandaging
was selected.
Ian recalled being daunted at
first, but eventually got used to
the bandages, resigning himself to
the fact that they were a ‘necessary
evil’. However, despite the use of
compression bandaging, the wound
continued to progress slowly, largely
due to ongoing issues with infection.
Suddenly, in January 2015 the wound
deteriorated significantly (
Figure 1
).
Wound assessment
The findings of wound and skin
assessment are presented in
Figure 1
.
Leg assessment
Ian’s limb was oedematous, which
would precipitate a change in his gait,
ability to mobilise and reduce the
effectiveness of the calf muscle pump,
and Doppler ultrasound to determine
his ankle brachial pressure index
(ABPI) revealed a reading within the
normal range of 0.8–1.3, making him
eligible for full compression.
The wound bed was covered with yellow slough, which
provides an ideal environment for bacterial growth and thus
should be debrided.
The wound’s appearance indicated that biofilm may be
present, and be a possible cause for the deterioration/delayed
healing of the wound.
The wound was producing a large volume of exudate, putting
Ian at increased risk of wound and skin breakdown.
The edge of the wound was typical for a venous ulcer, being
shallow and irregular in shape.
Some hyperkeratotic plaques were present secondary to
underlying oedema.
Figure 2.
Ian’s ulcer improved following compression bandaging and antibiotics.
Figure 1.
Findings of wound and skin assessment using the principles of TIMES.
T
I
M
E
S
Ian’s leg ulcer at presentation.