WOUND CARE TODAY
2016,Vol 3, No1
23
FOCUS ON NPWT
i
to seven days, although duration
may be less depending on the
wound type, size, rate or volume
of exudate, orientation of the
dressing, or environmental condition
(Payne and Edwards, 2014). The
same mechanisms of action apply
along with the same indications,
contraindications and precautions,
as described previously. These
systems have the advantage of a
smaller device which may be more
appropriate for some patients and
can be used to facilitate hospital
discharge, or step a patient down
from conventional NPWT. As the
wound progresses, the rationale
for use is largely dependent on
identified treatment goals.
Additional considerations before
use of disposable NPWT include:
i
Some single-use systems do
not have audible alarms. The
pump should be carried so that
it is accessible and the patient/
healthcare professional can check
the status routinely
i
Although they can be used under
clothing/bedding, it is important
that occlusive materials, e.g.
film dressings, are not applied
over the pad area of the dressing
as this will impair device
performance.
CONCLUSION
NPWT has been widely used to
benefit a large number of patients in
terms of both symptom management
and wound healing. Its ability to
simultaneously manage exudate,
i
Practice point
6LQJOH XVH GLVSRVDEOH 13:7
systems offer patients greater
ÁH[LELOLW\ DQG HQDEOH WKHP WR
FRQWLQXH ZRUN VRFLDO DFWLYLWLHV
ZKLOH VWLOO UHFHLYLQJ WKHUDS\
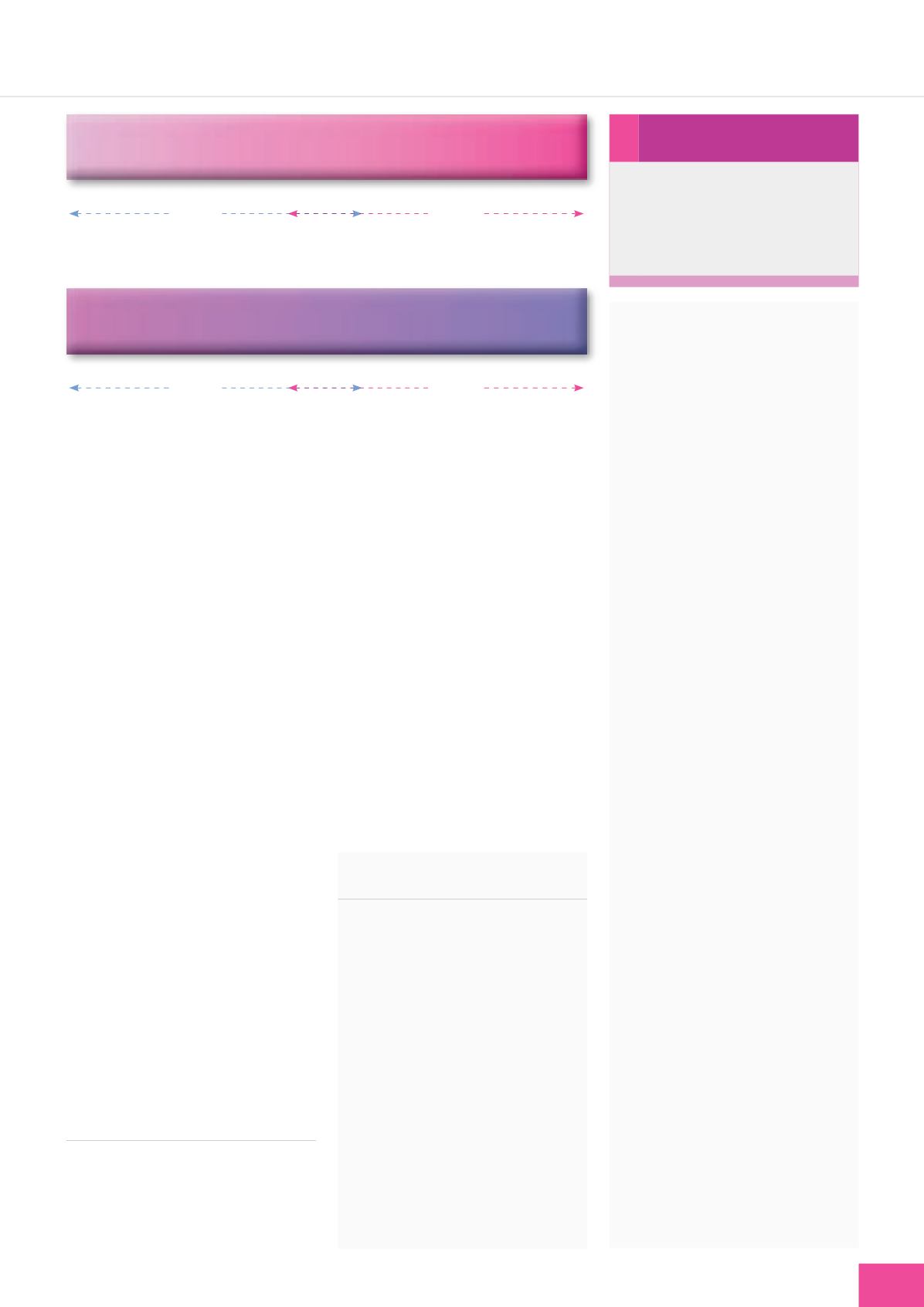
Lower pressure =
È
pain
Gauze
Foam
Higher pressure =
Ç
pain
Lower pressure =
È
exudate
Gauze
Foam
Higher pressure =
Ç
exudate
Figure 4.
Managing NPWT-related wound pain.
K, Maloney S, Sabo S (2010) NPWT
in everyday practice. Made Easy.
Wounds Int
1(5)
. Available online: www.
woundsinternational.com
Hurd T, Chadwick P, Cote J, et al (2010)
Impact of gauze-based NPWT on the
patient and nursing experience in the
treatment of challenging wounds.
Int
Wound J
7: 448–55
Malmsjö M, Borgquist O (2010) NPWT
settings and dressing choices. Made
Easy.
Wounds Int
1(3)
. Available online:
www.woundsinternational.comMalmsjö M, Ingemansson R, Martin R,
Huddleston E (2009) Wound edge
microvascular blood flow: effects of
negative pressure wound therapy using
gauze or polyurethane foam.
Ann Plast
Surg
63(6):
676–81
Malmsjö M, Lindstedt S, Ingemansson
R (2010) Effects of foam or gauze on
sternum wound contraction, distension
and heart and lung damage during
negative pressure wound therapy of
porcine sternotomy wounds.
Interact
Cardiovasc Thorac Surg
Dec 24
McCord SS, Naik-Mathuria BJ, Murphy
KM, et al (2007) Negative pressure
therapy is effective to manage a variety
of wounds in infants and children.
Wound Repair Regen
15(3):
296–301
Payne C, Edwards D (2014) Application
of the single use negative pressure
wound therapy device (PICO) on
a heterogenous group of surgical
and traumatic wounds.
Eplasty
.
Available online:
www.medscape.com/viewarticle/824485_4
Shultz G (2003) Wound Bed Preparation:
a systematic approach to wound
management.
Wound Repair Regen
11:
1–28
World Union of Wound Healing Societies
(WUWHS) (2008)
Principles of best
practice: Wound infection in clinical
practice. An international consensus
.
London: MEP Ltd
while promoting granulation tissue
is cited as the reasons for its use
with larger defects (Malmsjö and
Borgquist, 2010).
It is essential that clinicians
assess the patient and the wound
to optimise the use of the therapy.
The decision to use foam or gauze
interfaces should be based on
the individual patient and wound
assessment, and on the goals that
need to be achieved — whether
they be wound healing or symptom
management, or both. All clinicians,
patients and carers should know how
the system they are using works,
what the expected benefits of therapy
are and how these will be measured,
and what to do if there are any
suspected complications.
REFERENCES
Argenta LC, Morykwas MJ (1997)
Vacuum-assisted closure: a new
method for wound control and
treatment: clinical experience.
Ann Plast
Surg
563–77
Campbell PE, Smith GS, Smith JM (2008)
Retrospective clinical evaluation of
gauze-based negative pressure wound
therapy.
Int Wound J
5:
280–6
European Wound Management
Association (2007)
Position
document: Topical negative pressure
in wound management
. MEP Ltd,
London. Available online: www.
woundsinternational.com/pdf/
content_46.pdf
HendersonV, Timmons J, Hurd T, Deroo
WCT









