WOUND CARE TODAY
2016,Vol 3, No1
21
FOCUS ON NPWT
i
Remember:
When applying NPWT it is
important to consider the
SUHVVXUH VHWWLQJV W\SH RI
GUHVVLQJ XVHG DQG ZKHWKHU WKH
therapy is intermittent
RU FRQWLQXRXV
aetiologies, or those who have
compromised circulatory flow to
the wounded area
i
Burns – devitalised tissue must be
debrided before application
of NPWT
i
Patients with wounds in close
proximity to blood vessels,
delicate fascia, vital organs or
exposed tendons (ensure adequate
protection with overlying fascia,
tissue or other protective barriers)
i
Bone fragments or sharp edges
can puncture protective barriers,
vessels, or organs causing injury.
Any injury could cause bleeding,
which, if uncontrolled, could be
potentially fatal. It is important to
be aware of possible shifting of the
relative position of tissues, vessels
or organs within the wound that
might increase the possibility of
contact with sharp edges when
the dressing collapses. Sharp
edges or bone fragments must
be eliminated from the wound
area or covered to prevent them
from puncturing blood vessels
or organs before the application
of NPWT. Where possible,
completely smooth and cover any
residual edges to decrease the risk
of serious or fatal injury, should
shifting of structures occur. Use
caution when removing dressing
components from the wound so
that wound tissue is not damaged
by unprotected sharp edges
i
Enteric fistulae — ensure that
there is no distal obstruction. This
task should only be undertaken
with expert supervision
i
Patients receiving anticoagulant
therapy or platelet aggregation
inhibitors, or those who are
actively bleeding or have
weakened irradiated blood vessels
or organs. If significant bleeding
develops, immediately discontinue
the use of NPWT and take
measures to stop the bleeding.
Do not remove the dressing until
the treating clinician or surgeon
is consulted. Do not resume the
use of NPWT until adequate
haemostasis has been achieved,
and the patient is no longer at risk
of bleeding
i
Spinal cord injury — some
patients can experience autonomic
hyperreflexia (sudden elevation
in blood pressure or bradycardia
[slow heart rate] in response to
stimulation of the sympathetic
nervous system). Discontinue
NPWT to help minimise sensory
stimulation and seek immediate
medical assistance
i
Malnourished patients without
access to adequate nutrition/
nutritional supplements
i
Non-concordant patients.
WHICH WOUND-FILLER
MATERIAL
The function of the wound filler
is to deliver negative pressure to
the wound bed. The suction force
generated by the negative pressure
leads to active drainage of exudate
from the wound. No differences
in the mode of action have been
observed with either foam or gauze,
although polyurethane (PU) foam
results in more contraction than
gauze in large wounds (Malmsjö et
al 2010).
Choosing a filler
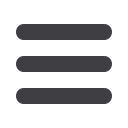
In the author’s clinical experience,
gauze fillers conform easily to the
shape and contours of the wound bed
during application and once negative
pressure is applied (
Figure 2
).
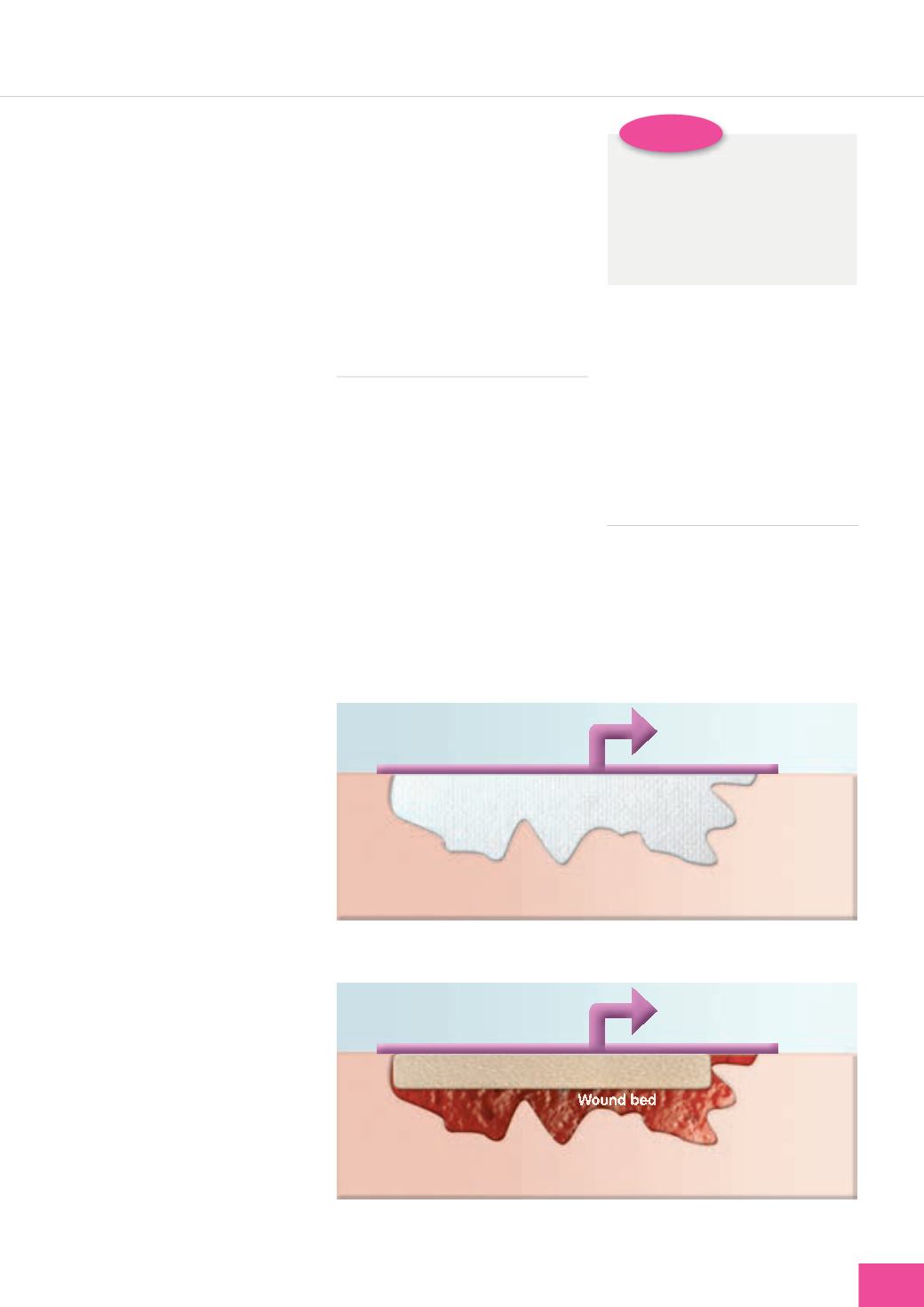
Conversely, foam does not
conform easily to non-uniform
wounds and needs to be cut and
shaped and layered to ensure it fits
the wound dimensions (
Figure 3
).
PRESSURE SETTINGS
The level of negative pressure may
be varied within the recommended
therapeutic range, according to
clinical circumstances (some of
which are outlined below), without
compromising clinical outcomes
and treatment goals (Campbell et al,
2008; Hurd et al, 2010;
Figure 4
).
Tubing attached to
suction source
Tissue
Tubing attached to
suction source
Tissue
Foam
Figure 2.
Gauze conforms easily to the shape and contours of the wound bed, giving
uniformity of pressure.
Figure 3.
Foam is easily applied to regular-shaped wounds, but fails to conform to
irregular-shaped wounds and would need to be cut.









