PALLIATIVE WOUND CARE
Top tip:
The patient’s comfort should
always take priority over any
wound care or measures to
prevent skin breakdown.
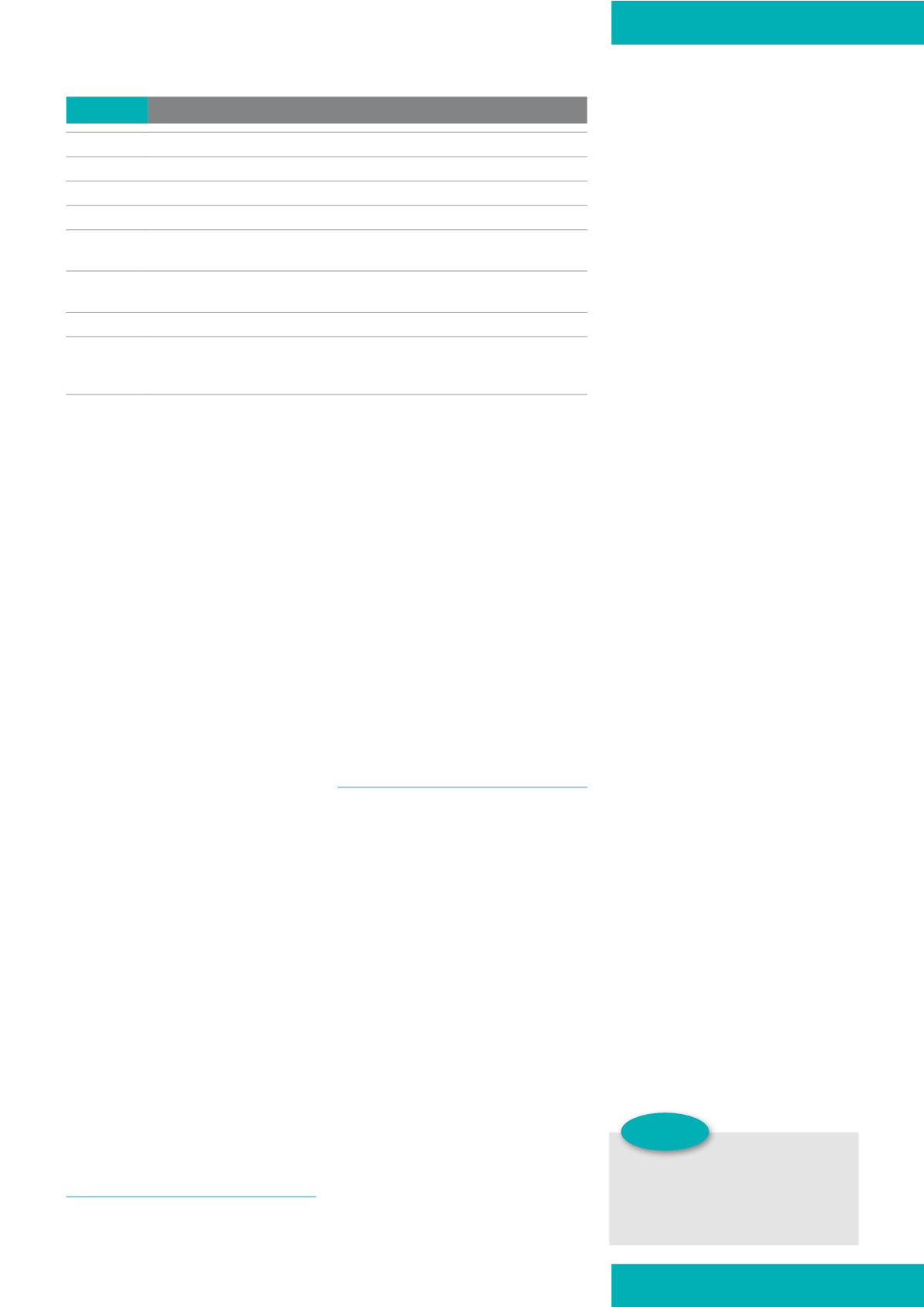
Table 1:
3ULQFLSOHV RI SDOOLDWLYH FDUH :RUOG +HDOWK 2UJDQL]DWLRQ >:+2@
`
It provides relief from pain and other distressing symptoms
`
It affirms life and regards dying as a normal process
`
It intends neither to hasten nor postpone death
`
It offers a support system to help patients live as actively as possible until death
`
It offers a support system to help the family cope during the person’s illness and in their
own bereavement
`
It uses a team approach to address the needs of patients and their families, including bereavement
counselling, if required
`
It enhances quality of life, and can also positively influence the course of the illness
`
It is applicable early in the course of illness, together with other therapies that are intended to prolong
life, such as chemotherapy or radiation therapy, and includes those investigations needed to better
understand and manage distressing clinical complications
JCN supplement
2015,Vol 29, No 5
15
[BDNG], 2012) (barrier products
are further discussed below under
‘maceration and excoriation’).
Radiotherapy burns, that can
occur in cancer patients, may be
helped by the application of gels
and specific foam products which
contain moisturisers (Princess
Royal Radiotherapy Team/St James’s
Institute of Oncology, 2011).
Pruritis, or itch, is sometimes
seen in palliative care. This skin
sensation can be distressing and
have a negative impact on quality of
life, with some patients even finding
pain preferable to pruritis (Zylicz,
2004). It is a difficult symptom to
manage and is largely unresponsive
to antihistamines. However, tricyclic
antidepressants may offer some
relief, while non-pharmacological
interventions, such as transcutaneous
electrical nerve stimulation (TENS),
are reported to offer some benefit
(Grocott, 2007).
Skin inspection should occur on a
daily basis, although changes noted in
the patient’s condition may increase
or decrease the frequency. All findings
from regular reassessment of the
patient’s skin should be documented
and form part of holistic care.
Educating patients and their families/
carers about the significance of skin
observation and reporting any redness
promptly is also vital to help prevent
skin breakdown (McManus, 2008).
WOUND MANAGEMENT
Care planning should be the result
of thorough patient assessment,
including psychological aspects,
and consider:
`
The patient’s personal history,
social circumstances
and understanding
`
Clinical assessment, i.e. the
patient’s illness, symptoms,
treatment and current
management
`
Wound assessment, i.e. the
site, size, tissue types present,
condition of the wound bed and
periwound skin, exudate, pain,
odour, and bleeding
`
The family’s/carer’s concerns,
expectations, etc
`
The patient’s wishes, concerns
and priorities.
WOUNDS TYPES
In the author’s clinical experience,
the two main categories of wounds
encountered in palliative care are
pressure ulcers and malignant wounds.
Pressure ulcers
Patients with palliative care needs
are at significant risk of developing
pressure ulcers (Stephen-Haynes
2014) as a result of:
`
Increased age
`
Reduced mobility and activity
`
Poor nutritional status
`
Exposure to friction and shear
`
Exposure to moisture (Langemo
et al, 2010).
Prevention of pressure ulceration
includes risk assessment, re-
positioning, nutritional assessment/
management, continence
management and the use of pressure-
relieving equipment, including
bed-bases, mattresses and cushions,
to help minimise the negative impact
that having a pressure ulcer can have
on the patient’s physical, emotional
and social life (European Pressure
Ulcer Advisory Panel/National
Pressure Ulcer Advisory Panel/
Pan Pacific Pressure Injury Alliance
[EPUAP/NPUAP/PPPIA], 2014;
National Institute for Health and
Care Excellence [NICE], 2015).
Malignant wounds
Malignant wounds are caused
by the invasion of skin tissues
and supporting blood and lymph
vessels by cancer cells (Pearson and
Mortimer, 2004). These may be:
`
Locally advanced
`
Metastatic
`
Recurrent.
As the tumour extends, the
angiogenesis development of
the blood capillaries becomes
disordered altering the blood clotting
mechanism within the tumour
(Collier, 2000).
Grocott (2007) observed that
primary cancers such as breast, head,
neck, colon and penis more commonly
fungate. Fungating breast cancer can
appear as deep necrotic ulceration
with proliferative growth of the ulcer
margins, while cancer of the ovary,
caecum and rectum, which infiltrate
the anterior wall of the abdomen,
present as small raised nodules,
developing into necrotic‘cauliflower-
like’structures (Grocott, 2007).
It is essential that care includes
treatment of the underlying tumour,
management of comorbid conditions,
and symptom management.
Specific aspects relating to tissue
viability in palliative wound care
include maceration and excoriation,
malodour, infection, bleeding
and pain.
Maceration and excoriation
The nature of wounds occurring









