52
SKIN CARE TODAY
2015,Vol 1, No 1
FOCUS ON VENOUS ECZEMA
i
eczema fails to respond adequately
to treatments and deeper skin
changes develop. Recurrent
episodes and persistent venous
insufficiency can progress to the
chronic form of venous eczema,
lipodermatosclerosis (NICE, 2012a;
Morton and Phillips, 2013).
Lipodermatosclerosis charac-
teristically has areas of ‘atrophie
blanche’ due to dermal fibrosis,
sclerosis and fat necrosis, as well as
permanent skin pigment changes
(red, purple, brown and white).
The skin tissue becomes very dense
and tight leading to restricted
movement in the ankle and lower
leg. The erythema varies in severity
and can be intensely pruritic. Due
to changes in skin architecture,
the lower leg takes on the classic
diagnostic shape of an up-turned
champagne bottle and is susceptible
to injury. Itch and pain are the most
commonly reported symptoms,
which result in skin trauma, ulcer
formation and failure to heal
(Champion et al, 1998; Walsh and
Santa Cruz, 2010; NICE, 2012a;
Morton and Phillips, 2013).
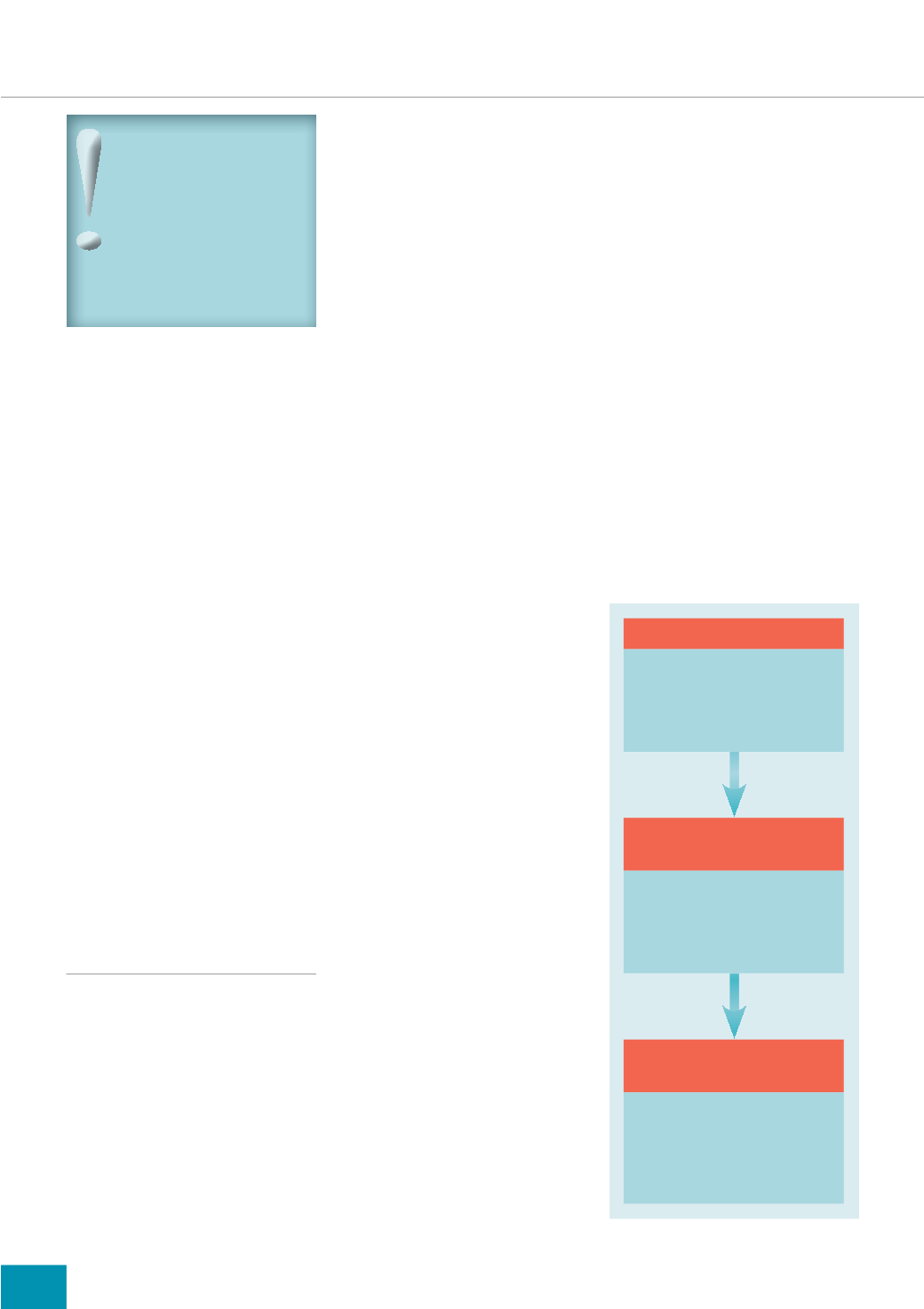
MANAGEMENT STRATEGIES
Early intervention and treatment
of venous eczema is vital, as
progression of the condition can
lead to profound psychological and
physical morbidity, especially if
venous insufficiency progresses and
ulcer formation occurs (Middleton,
2007). The principles of care for
venous eczema are as follows
(
Figure 3
):
1. Manage the underlying
condition (venous insufficiency)
2. Manage the condition
(venous eczema)
3. Manage any complications
(itch, pain, infection, contact
dermatitis/allergy, psychological
morbidity.
Holistic assessment
Patient-centred care demands
holistic needs assessment which
comprises addressing the physical,
cognitive, emotional, spiritual,
financial and social aspects of the
condition (Nursing and Midwifery
Council [NMC], 2007).
As it is a chronic progressive
condition, people with venous
eczema may have to consider
lifestyle changes which support
medical and nursing management.
Taylor (2012) advocates using a
holistic tool for the elderly which
addresses the following domains:
physical health, mental health and
emotional wellbeing, awareness
and decision-making, medicines
management, communication
and sensory functioning, walking
and movement, personal care and
daily tasks, living arrangements
and accommodation, relationships,
work, finance and leisure.
In addition to the above
domains, as part of holistic care,
spiritual and religious needs of
patients require assessment — this
involves discussing a patient’s
religious and spiritual beliefs,
wishes, expectations and how these
impact on his/her life and wellbeing
(Ledger, 2005).
Holistic needs assessment is vital
to the success of any intervention,
as patients’ expectations and
understanding should be
considered. The epidemiology of
chronic venous disease and venous
eczema indicates patients are likely
to be in mid-life or elderly, with
increased body mass index (BMI)
and reduced mobility. Therefore,
nursing assessment needs to
address the patient’s knowledge
and understanding of the condition,
social implications, activities of
daily living, financial implications
and emotional reactions.
The quality of life of patients
with CVD can be severely affected
due to itch, pain, immobility, social
isolation, anxiety and depression
(Middleton, 2007; Guanella and
Kahn, 2012; Sritharan et al, 2012;
Sanchez et al, 2013). The use of a
holistic needs assessment and a
quality of life assessment tool, such
as the Dermatology Life Quality
Index (DLQI), will facilitate a patient-
centred approach and improve any
medical or nursing intervention,
maximising patient experiences and
outcomes (Findlay and Kahn, 1992).
Clinical assessment of vascular
disease is advocated to inform
decision-making when managing
venous eczema. In the UK, the CEAP
(Clinical, Etiological, Anatomical
and Pathophysiological signs)
scoring system is used for clinical
assessment of venous disease and
categorises venous eczema as C4a
and lipodermatosclerosis as C4b
(Eklof et al, 2004).
Did you know:
9HQRXV HF]HPD LV DOVR
NQRZQ DV JUDYLWDWLRQDO
HF]HPD YDULFRVH HF]HPD
DQG VWDVLV HF]HPD ,W
LV QRZ UHJDUGHG DV D
FXWDQHRXV PDQLIHVWDWLRQ RI
YDVFXODU LQVXIÀFLHQF\ 0RUWRQ
DQG 3KLOOLSV
3ULQFLSOHV RI FDUH
i
Manage the underlying
condition
i
Manage the venous eczema
i
Manage any complications
3ULPDU\ FDUH
DVVHVVPHQW
i
Holistic needs assessment
and quality of life
i
Vascular disease assessment
i
Skin assessment
&RPPXQLW\ QXUVH
PDQDJHPHQW
i
Emollient therapy
i
Corticosteroid therapy
i
Compression hosiery
i
Psychosocial support
Figure 3.
Venous eczema pathway of care.