standards for atopic eczema in
children (NICE, 2013) (which were
themselves based on the groundwork
done in the previous 2007 guidelines).
These latest 2013 quality standards
distil the 86 recommendations
from the earlier guideline
into a much easier-to-digest
seven statements. As the only
patient representative on
both the NICE guideline and
quality standard for childhood
eczema, the author reflects on
the details behind the seven
statements and the impact they
can have on childhood eczema.
Each of the quality statements
below is accompanied by
some background; specific
recommendations and, where
applicable, an illustrative comment
from someone in the NSGCCE
community.
QUALITY STANDARD
STATEMENT 1
Children with atopic eczema should be
offered, at diagnosis, an assessment that
includes recording their detailed clinical
and treatment histories and identification
of potential trigger factors.
Generally, eczema is diagnosed and
FOCUS ON CHILDHOOD ECZEMA
i
58
SKIN CARE TODAY
2015,Vol 1, No 1
E
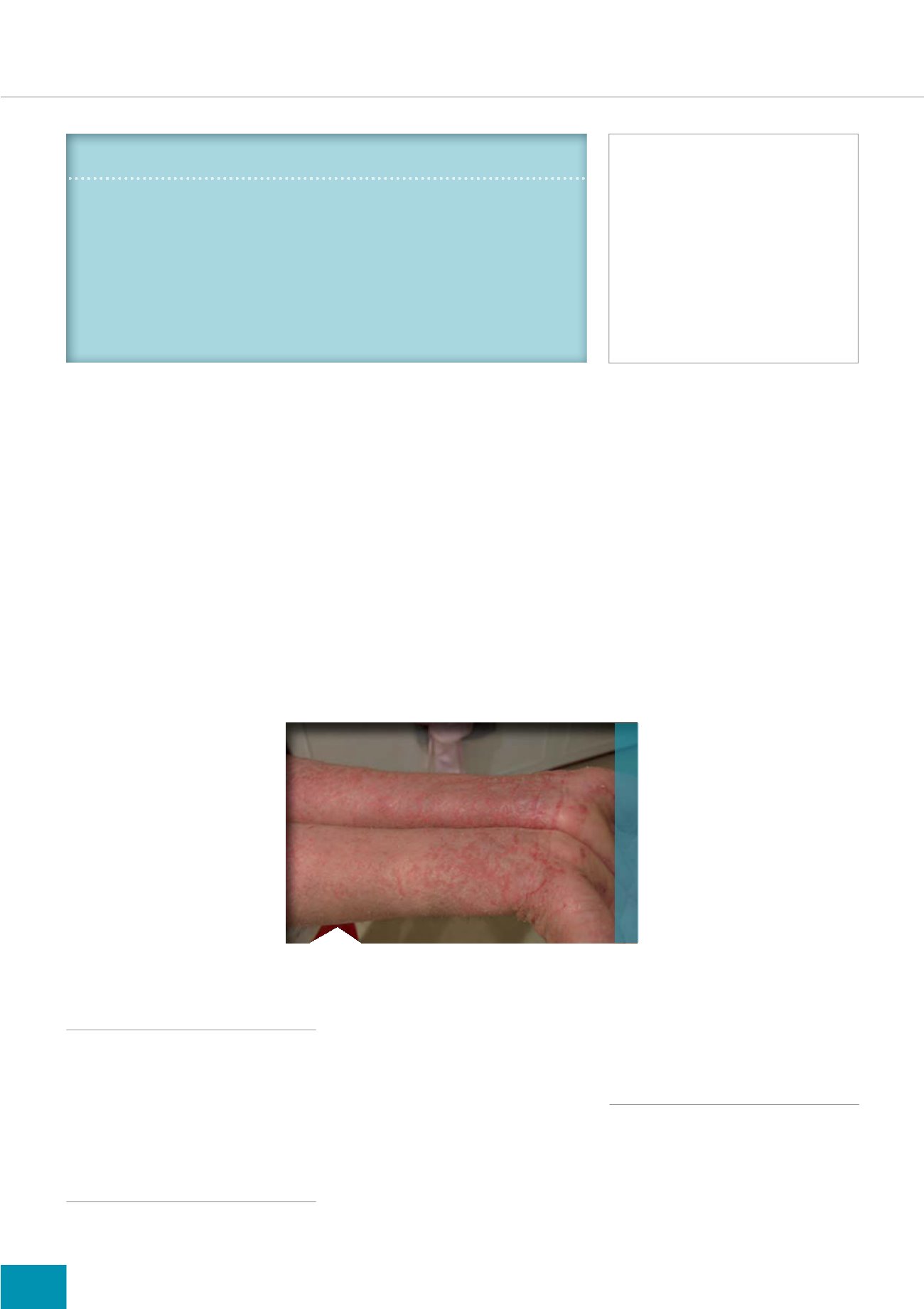
czema (also called atopic
dermatitis or atopic eczema)
is one of a group of related,
inherited conditions that also includes
asthma, food allergy and hay fever. It
makes the skin dry, itchy, red, broken
and sore (
Figure 1
) and there
are clear diagnostic criteria
(National Institute for Health
and Care Excellence [NICE],
2007) (
Table 1
).
Twenty percent of children
in the UK will have some
experience of eczema, and it
remains the most common skin
condition in children of primary
school age or under. Sixty
percent of these children will
find that their eczema improves
over time (Hoare et al, 2000).
BACKGROUND
In writing this article, the author who
has eczema, reflects on the quality
standard for childhood eczema
(NICE, 2013).
How do current childhood eczema
standards influence practice?
Amanda Roberts has eczema herself and is
involved with the Nottingham Support Group for
Carers of Children with Eczema (NSGCCE)
IN BRIEF
7ZHQW\ SHUFHQW RI FKLOGUHQ LQ WKH 8. ZLOO KDYH VRPH H[SHULHQFH RI
HF]HPD ,W UHPDLQV WKH PRVW FRPPRQ VNLQ FRQGLWLRQ LQ FKLOGUHQ RI
SULPDU\ VFKRRO DJH RU XQGHU
(F]HPD LV RQH RI D JURXS RI UHODWHG LQKHULWHG FRQGLWLRQV WKDW DOVR
LQFOXGHV DVWKPD IRRG DOOHUJ\ DQG KD\ IHYHU
,W FDQ OHDYH WKH VNLQ GU\ LWFK\ UHG EURNHQ DQG VRUH DQG LI
XQWUHDWHG FDQ OHDG WR VLJQLÀFDQW GLVFRPIRUW DQG TXDOLW\ RI
OLIH LVVXHV
KEY WORDS:
(F]HPD
&KLOGUHQ
6NLQ GDPDJH
6WHURLGV
(PROOLHQW WKHUDS\
6NLQ SURWHFWLRQ
Amanda Roberts
Author’s experience
Unfortunately, the author was a child
who did not‘grow-out’of eczema
(or asthma). In due course, she had
children (who both have eczema)
and subsequently became involved
Figure 1.
Eczema on a patient’s arms and hands.
.
Credit: Jambula at en.wikipedia
with the Nottingham Support Group
for Carers of Children with Eczema
(NSGCCE), an organisation that
provides information for carers of
children with eczema. The NSGCCE
is mainly web-based and run jointly
by a team of healthcare professionals
from the dermatology department
at Nottingham University Hospitals
NHS Trust and carers of children
with eczema.
Guidelines
In September 2013, NICE published