42
WOUND CARE TODAY
2017,Vol 4, No 1
FOCUS ON
E
DGE
i
Remember:
Epithelial advancement is a
clear indication that a wound
is healing.
result in reduced perfusion, which
damages surrounding tissues and
prevents the creation and attachment
of new skin cells (Dowsett and
Newton, 2005; Leaper et al, 2012).
TREATMENT
To promote wound edge progression,
clinicians must establish a differential
diagnosis and offer treatment
that addresses the underlying
cause of the wound, for example,
correcting venous hypertension with
compression in patients with venous
ulceration (O’Meara et al, 2012;
Ashby et al, 2014 ), or offloading of
the diabetic foot. Furthermore, it is
essential that the chosen treatment
addresses local wound symptoms
identified in
Table 1,
as otherwise
patients may struggle to concord with
treatment (Price, 2013).
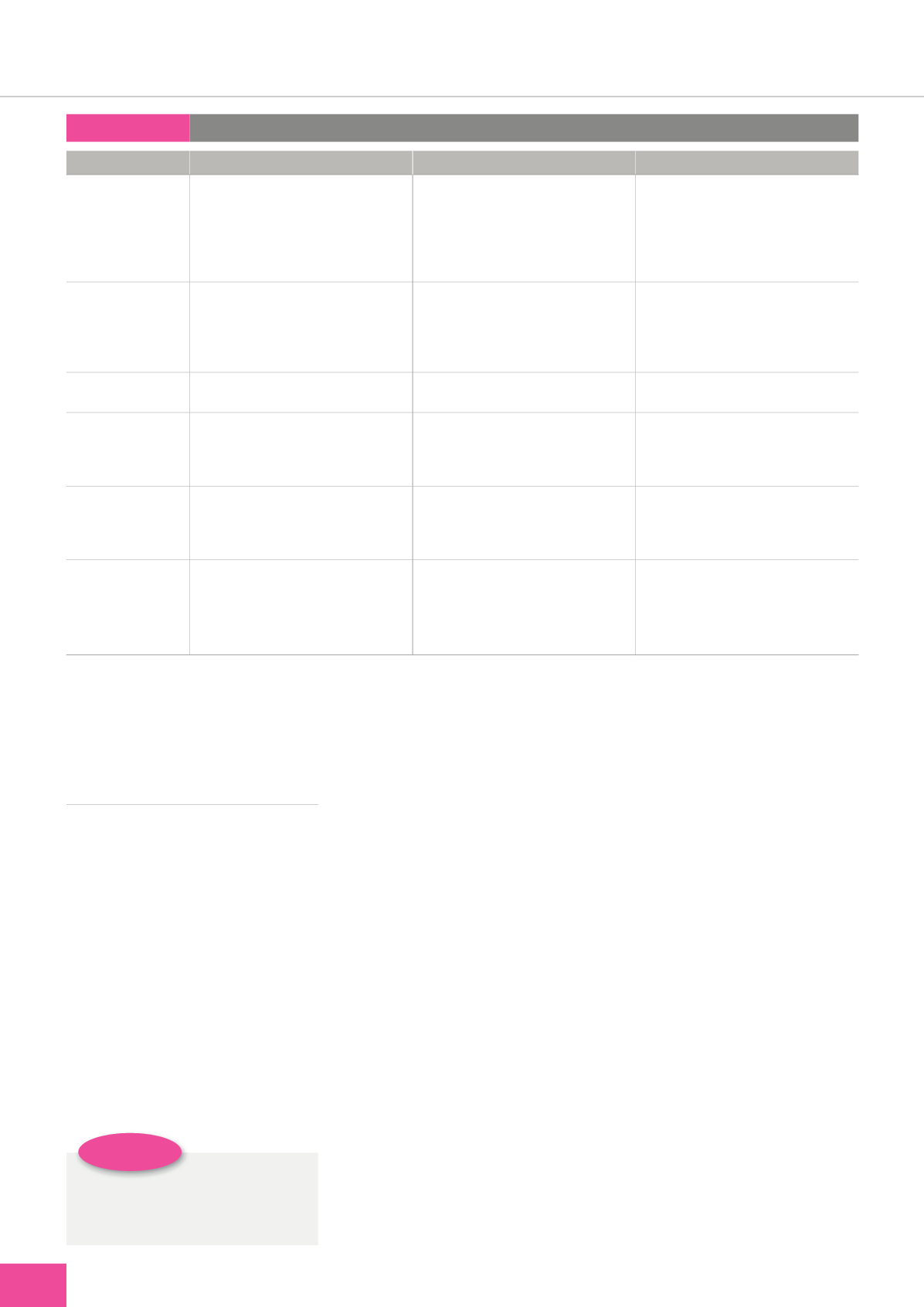
Table 1:
Clinical presentation
Clinical presentation
Description
Clinical impact
Treatment options
Maceration
Environmental damage from excess volume
of exudate left on the periwound skin, as the
enzymes break down the stratum corneum
Periwound extension
Inflammation
Skin susceptible to damage from trauma
Exudate management
Treatment that addresses the underlying cause of
the wound and thereby minimises the volume
of exudate
Compression
Absorbent dressings
Excoriation
Environmental damage/loss of skin from abrasion Inflammation
Pain
Skin susceptible to damage from trauma or skin
stripping from exudate and adhesives
Skin protection with barrier products, adhesive
removers/silicone adhesives
Papillomatosis
Skin surface elevation caused by hyperplasia and
enlargement of the dermal papillae
Reduced hydration and inelasticity
Diagnosis of underlying condition
Emollients to maintain elasticity and hydration
Hyperkeratosis
Thickening of the stratum corneum (outermost
layer of skin) secondary to chronic inflammation
Excess development of the stratum corneum or
delayed exfoliation
Dryness
Fissures
Diagnosis of the underlying condition
Debridement cloths
Emollients
Callus
Localised thickening of the epithelium because of
pressure or friction
Increases pressure
Can lead to sub-callous ulceration
Prevents accurate assessment
Prevents epithelial migration
Offloading
Sharp debridement
Eczema/dermatitis
Irritation of the skin secondary to inflammation,
caused by underlying pathology or application
of allergens
Erythematous, small blisters, weeping and crusting
Often itchy
Can lead to scratching and hyperkeratosis
Diagnosis of the underlying cause
Treatment targeted at underlying pathology
Avoid common irritants
Simple emollients to rehydrate the skin
Topical corticosteroids
It is common for patients to be
labelled as non-concordant when,
in fact, it is the clinician’s failure to
address symptoms, i.e. successful
diagnosis of the type of wound pain
and its management, or breaking the
itch–scratch cycle associated with
periwound eczema.
Critical to success is concomitant
treatment of underlying conditions
that negatively impact on healing —
often termed, optimising the host.
Examples of this may be addressing
nutritional deficiencies to achieve tight
glycaemic control and/or managing
underlying conditions, e.g. diabetes,
heart failure, autoimmune disorders,
that impact on the host immune
system. In tandem, prevention
of complications associated with
wounds, such as infection, excoriation
or maceration, is critical for patient
concordance and achieving positive
outcomes. Unfortunately, misdiagnosis
or having treatment for a wound of
unknown origin is not uncommon
(Drew, 2007; Guest et al, 2015; 2017).
Damaged periwound skin is
common in chronic wounds. It has
been linked to delayed healing, pain
and discomfort, and failure to address
issues can lead to extension of the
wound margins (Ousey and Cook,
2011). Thus, clinicians should protect
the periwound skin, establish the
correct cause and plan corrective care,
for example, minimising contact with
moisture or rehydrating dry tissue with
emollients. Managing excess exudate
is vital if clinicians want to reduce
the risk of periwound skin damage
(Dowsett et al, 2015). Excess moisture
can affect the barrier function of the
skin and is linked to continued skin
breakdown, maceration and dermatitis.
Chronic wound exudate is high in pro-
inflammatory mediators, and it alone
can be a wounding agent (Schultz et
al, 2003; Leaper et al, 2012).
Addressing the‘T’(tissue non-
viable) of TIME in relation to the use
of debridement of devitalised skin,
callus, necrosis and slough is also a key
component of encouraging migration
of the edge of the wound. Periwound
callus and scabs, i.e. hard plaques
of skin, can cause pressure when
the patient is walking or beneath
compression, and, as such, should be