34
WOUND CARE TODAY
2015,Vol 2, No 1
FOCUS ON PRESSURE ULCERS
i
(NPUAP/EPUAP/PPPIA, 2014):
i
Full medical history
i
Nutritional assessment
i
Pressure ulcer
risk assessment
i
Details of any pressure-
relieving equipment in use
i
Ability of patient
to reposition
i
Environment
i
Pain
i
Pressure ulcer assessment.
An assessment of the
pressure ulcer itself takes
place following the holistic
assessment (see below). The
findings of both of these
assessments should form the
basis for the most appropriate
management plan (NPUAP/
EPUAP/PPPIA, 2014).
The wound
Once a holistic assessment has
been completed it is important to
undertake a thorough assessment of
the ulcer itself. This should include
a thorough wound assessment,
incorporating the following
elements:
i
Wound location
i
Category
i
Size
i
Any tunnelling and undermining
i
Wound edges
i
Condition of surrounding skin
i
Exudate
i
Odour
i
Pain.
Although all the above should be
included in a wound assessment it
is beyond the scope of this article to
discuss them all in detail, however
some items are crucial.
Location
Knowing where the ulcer is will
help with treatment and dressing
selection. For example, eschar on the
sacrum may require debridement;
whereas eschar on the heel is often
left in place as poor vascular supply
to the lower limb can mean that
debriding may create a larger wound
that will not heal (Suzuki, 2009).
Similarly, a dressing suitable for
the sacrum may not be suitable for
the heel and
vice versa
. Knowing
the location of the wound will also
assist with the selection of the most
skin assessment is very
important. The HSCIC (2015)
define a ‘new’pressure ulcer
as being a pressure ulcer that
developed 72 hours or more
after the patient was admitted
— therefore documenting
any skin discolouration can
be crucial to establishing this.
It is also important to follow
the pressure ulcer categories
contained in any local policies.
ASSESSMENT
To provide an appropriate
treatment plan, it is vital that the
management of any pressure
damage begins with a holistic
assessment of the patient, including
Table 1:
'L;HUHQWLDWLRQ EHWZHHQ PRLVWXUH OHVLRQV DQG SUHVVXUH
XOFHUV DGDSWHG IURP 'HÁRRU HW DO
0RLVWXUH OHVLRQ
3UHVVXUH XOFHU
Cause
i
Moisture must be present,
e.g. shining, wet skin caused by
urinary incontinence or
loose stool
i
Pressure and/or shear present
Location
i
A lesion not over a bony area is
unlikely to be a pressure ulcer
i
A lesion that is limited to the
anal cleft only and has a
linear shape
i
Peri-anal redness/skin
irritation is most likely to be
due to faecal irritation
i
Tends to be located over a
bony prominence
i
Limited to one spot
Shape
i
Diffuse: different
superficial spots are more likely
to be moisture lesions
i
In a kissing ulcer (copy lesion),
at least one of the wounds is
likely to be caused by moisture
i
Circular shape or with a
regular shape (with the
exception of friction damage)
Depth
i
Superficial (partial skin loss)
i
In cases where infection is
present, the lesion can deepen
i
Partial-thickness skin loss:
only the top layer of skin
damaged (category two)
i
Full-thickness skin loss: all
layers of the skin are damaged
(category three or four)
Necrosis
i
There is no necrosis in
moisture lesions
i
A black necrotic scab over
a bony prominence indicates
a category three or four
pressure ulcer
Edge
i
Often have diffuse or
irregular edges
i
Edges are distinct
Colour
i
If the redness is not uniformly
distributed it is likely to be a
moisture lesion
i
If the surrounding skin is
white it may be macerated due
to excessive moisture
i
Red skin non-blanching
(category one)
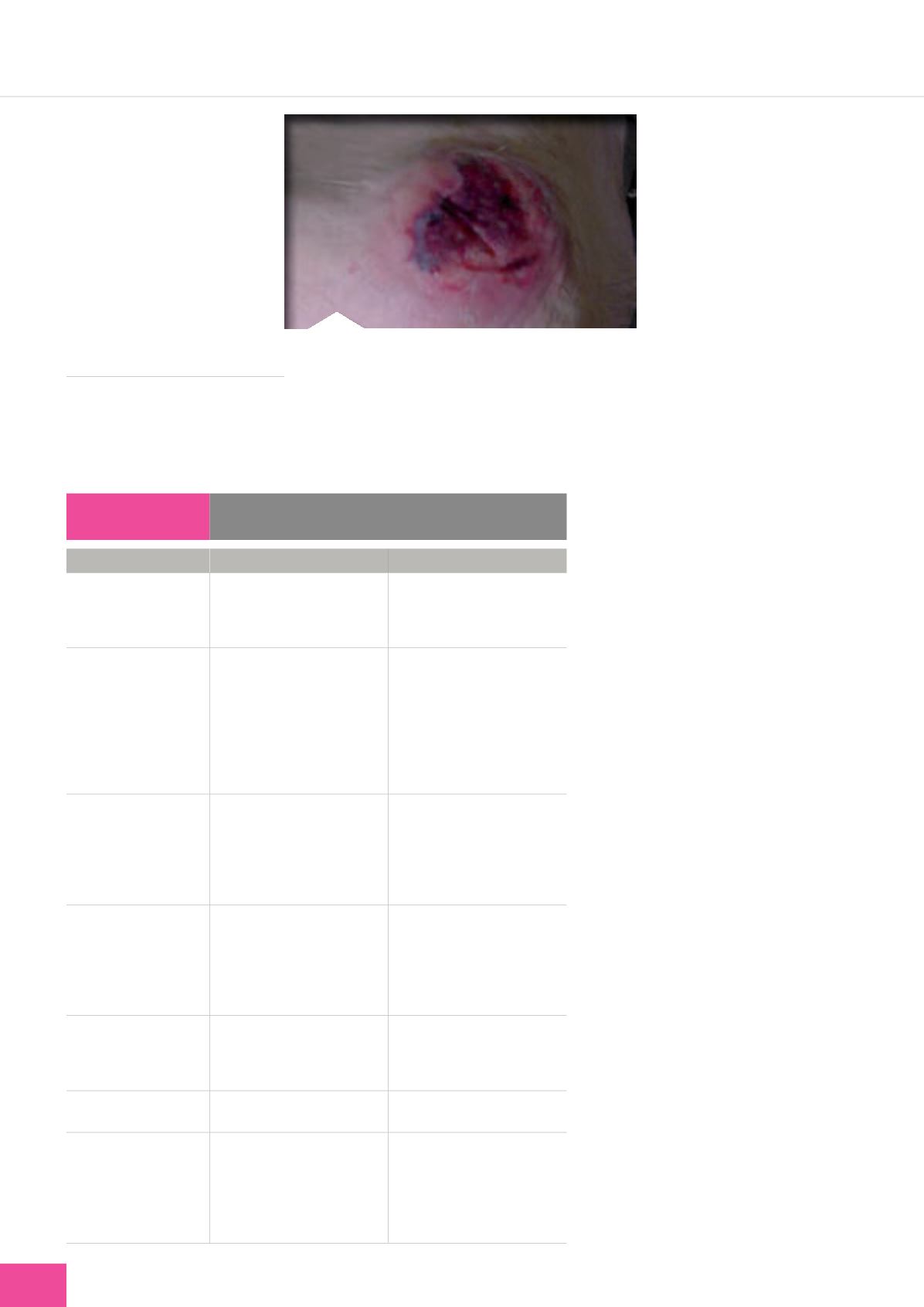
Figure 3.
An example of bruising that is likely to con-
stitute deep tissue injury.This should be photographed
and recorded as per local policy. Any other bruising not
associated with pressure areas, e.g. on the forearms or
legs, should not be recorded as a pressure ulcer.