SKIN CARE TODAY
2016,Vol 2, No 1
21
FOCUS ON ATOPIC ECZEMA
›
TOPICAL STEROIDS
Topical steroids are effective
in reducing the symptoms of
inflammation through their anti-
inflammatory, immunosuppressive,
antiproliferative and vasoconstrictive
actions (Ersser andVan Onselen,
2010). Topical steroid preparations
are available in lotion, cream,
ointment, gel, impregnated tape
and mousse form, and in four
different strengths:
›
Mild
›
Moderate
›
Potent
›
Very potent.
Application should be performed
in conjunction with a good
moisturising regimen to enhance
absorption, efficacy and ease of
application. Topical steroids should
be applied 30 minutes after applying
a moisturiser to avoid diluting the
steroid (BDNG, 2012).
Topical application is once-daily
(Scottish Intercollegiate Guidelines
Network [SIGN], 2011), with the
strength of the steroid tailored to the
severity, age and site of the eczema
(Primary Care Dermatology Society
[PCDS], 2015).
A step-up and step-down
approach is recommended (NICE,
2007), which matches the strength of
topical steroid to the severity of the
eczema — once the eczema settles,
the strength of steroid is decreased,
rather than being withdrawn
altogether. If the eczema then
flares-up again, the strength can be
stepped-up (NICE, 2007).
The use of a ‘steroid ladder’
aids the identification of steroid
strength and a stepped-approach
to treatment (Page and Robertson,
2004). The steroid ladder groups
the topical steroids according to
their strength —‘very potent’,
‘potent’,‘moderate’ and ‘mild’— for
ease of identification. The theory is
illustrated as a step ladder to advise
the user to ‘step-up or down’ the
ladder but not to ‘jump off’. In other
words, it reminds patients to reduce
the strength of steroid rather than
ceasing treatment.
As a general rule, a weak
preparation should be used on the face
and genital areas, with a moderate or
potent steroid applied elsewhere on
the body (Baron et al, 2012).
The amount of corticosteroid is
measured in finger-tip units (FTUs),
which comprise the distance from
the tip of the adult index finger to
the first joint. One finger-tip unit will
adequately treat the surface area of two
adult palms (Long and Finlay, 1991).
For frequent eczema flares, it
is suggested that a potent topical
steroid be applied to areas of
inflammation once-daily for two
weeks, then on alternate days for two
weeks (PCDS, 2015). Once benefit
is seen, the potency of steroid is
reduced until they are discontinued.
As with moisturisers, steroid
ointment preparations are preferable
to creams due to the lack of stinging
pain on application, which can
enhance concordance (Baron et al,
2012). However, creams are advised
in‘weepy’ eczema (exhibiting
exudate), due to their more effective
drying action (see ‘Top tips on topical
corticosteroid use’,
pp 33–35
).
A clear care plan will enhance
understanding and concordance
with treatment, both in patients, but
also in staff where different nurses
might be involved in treatment, for
instance. This is particularly relevant
as fears about using topical steroid
therapy (due to its strength) can often
lead to under-treatment, subsequent
treatment failure and disillusionment
(Smith et al, 2010).
Nurses should take time to
thoroughly explain the benefits of
topical treatments and formulate
a treatment plan that fits into the
patient’s daily life. A demonstration
of the amount of topical treatment
to apply to certain areas, along
with application techniques, can
improve patient confidence. Written
information can also help patients’
understanding and concordance with
treatment regimens.
TOPICAL CALCINEURIN
INHIBITORS
Topical calcineurin inhibitors are
immuno-modulating agents licensed
for the treatment of atopic eczema
(BMA/RPS, 2013). Their main benefit
is that they are not steroid-based and
do not cause skin atrophy. They are
considered if topical steroid treatment
has failed or where there is a risk of
adverse effects from further topical
steroid use (NICE, 2004). Treatment
is usually initiated by a dermatologist
(BAD, 2013).
Topical calcineurin inhibitors
include creams and ointments
incorporating tacrolimus and
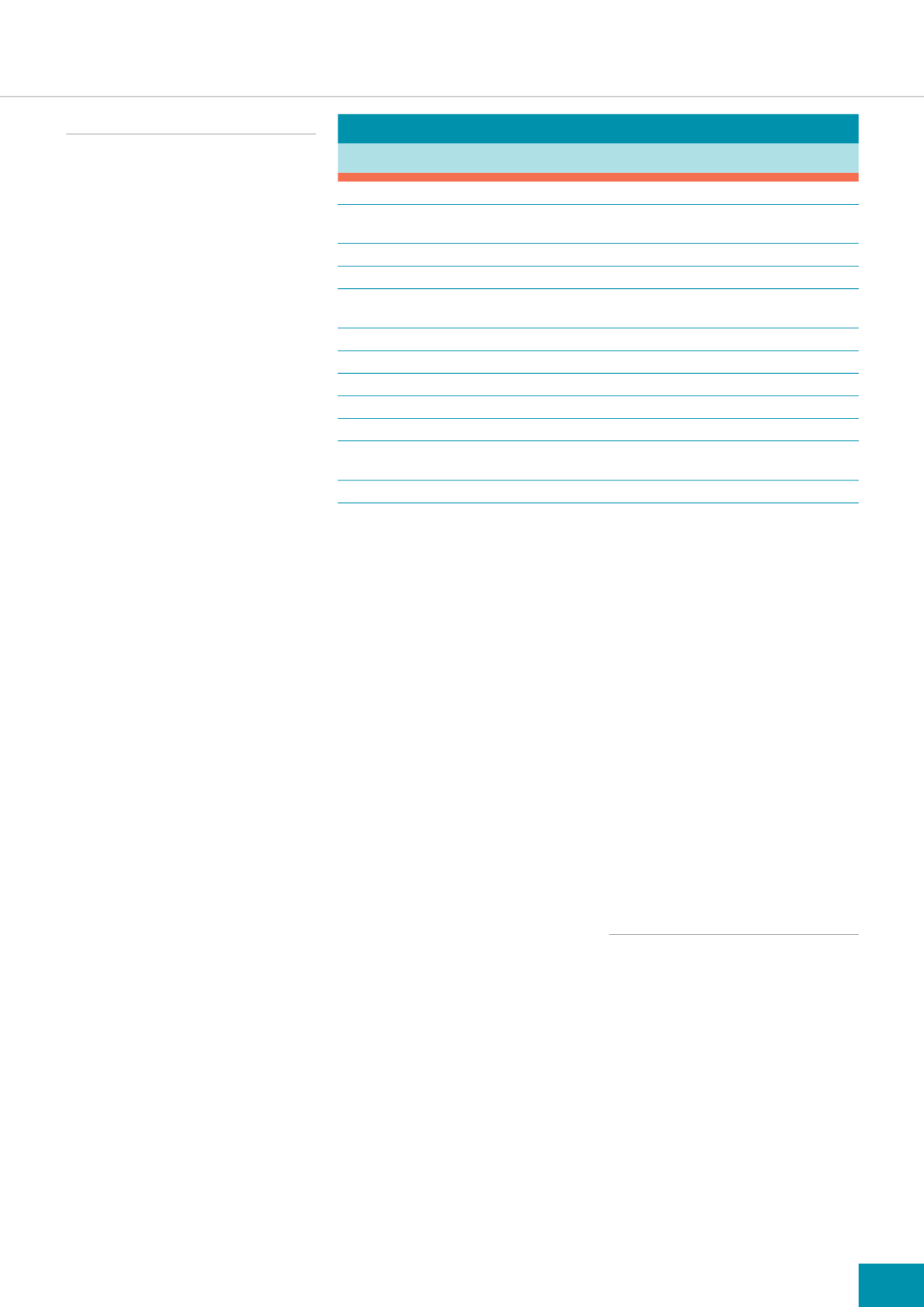
Table 1:
Practical tips for application of emollients (BDNG, 2012)
Use complete emollient therapy, comprising bath additives, soap substitutes and leave-on emollients
Bath oils can be added to the bath water or applied directly to damp skin as a soap substitute in the shower
or bath and then rinsed off
Apply liberal amounts of topical leave-on moisturisers — approximately 500–600g per week
Apply leave-on moisturisers throughout the day
Always apply emollients in a downward motion following the direction of the hair to avoid folliculitis
and excess rubbing
Use emollients directly after a bath/shower
Creams should be applied to‘weepy’skin
Greasy ointments are best applied to dry, scaly, lichenified and/or fissured skin
Do not stop emollients when eczema resolves. A daily emollient routine can help prevent flares
Always remember that the best emollients are the ones patients like, as they are more likely to apply them
To prevent moisturisers becoming contaminated, use clean implements to scoop products out of tubs or use
sealed pump dispensers
Warn patients that paraffin-based products are flammable









