SKIN CARE TODAY
2017,Vol 3, No 1
23
FOCUS ON ATOPIC ECZEMA IN CHILDREN
i
Nevertheless, when eczema
does not respond to emollient
therapy, it will require a step up in
management and the introduction
of topical corticosteroids.
Depending on the severity, the
stepped approach may also include
topical calcineurin inhibitors,
bandages and phototherapy. In
more severe cases, where the
condition is uncontrolled or exhibits
signs of erythoderma (generalised
acute redness) (Oakley, 2016),
paediatric dermatologists may
consider using a systemic therapy,
usually oral medication that is
absorbed into the bloodstream.
Oral corticosteroids and
immunosuppressant drugs are
normally used and aim to improve
skin barrier function and reduce
inflammation by suppressing the
immune response, which will
hopefully control intensive pruritus
(BAD, 2016).
Topical corticosteroids and
calcineurin inhibitors
Topical corticosteroids are an
anti-inflammatory medication in
the form of a cream or ointment.
Steroids are hormones that occur
naturally in the body and are key
to the immune response — steroid
medications are manufactured
versions of these natural hormones.
Topical corticosteroids work
by altering the manifestation
of cytokines (cells involved in
inflammation), thereby reducing
inflammation in the management
of moderate-to-severe eczema
when applied directly onto the skin
(Mehta et al, 2016). In addition,
they have an antiproliferative and
vasoconstrictive effect.
Topical corticosteroids can
be combined with antibacterial
or antifungal agents that are
prescribed for the management
of eczema in children, particularly
on the face (Oakley, 2016). Topical
corticosteroids are prescribed for a
limited period of time, normally 1–6
weeks and are used in combination
with an emollient regimen. The
purpose of this approach is to
control the flare and to obtain
remission from acute flare (Peterson
and Chan, 2016).
When treating children with
moderate-to-severe eczema, it
is recommended that treatment
should be initiated with a lower
strength corticosteroid to prevent
side-effects such as skin atrophy
and hyperpigmentation, particularly
on the face and the flexural skin
(Walling and Swick, 2010).
Due to potential side-effects,
parents and carers are often
reluctant to use this type of
treatment, therefore, education on
the risks and benefits is important.
Nurses should use a standard
recommended method known as
the fingertip unit (FTU) to measure
the necessary amount of topical
steroid that should be used on
an active skin area (
Figure 2
). In
essence, one FTU represents the
amount of topical steroid that
should be squeezed from the tube
onto an adult’s fingertip. This area
ranges from the tip or end of the
index finger down to the first crease
of the finger.
Topical calcineurin inhibitors
are used particularly in recurrent
eczema flares on the face, groin
and neck, replacing the topical
corticosteroid therapy in children
over two years old. They are
composed of immune-modulator
and anti-inflammatory agents,
which are very effective in
Red Flag
Eczema herpeticum
(F]HPD KHUSHWLFXP LV D YLUXV
that deteriorates rapidly and
may lead to hospital admission.
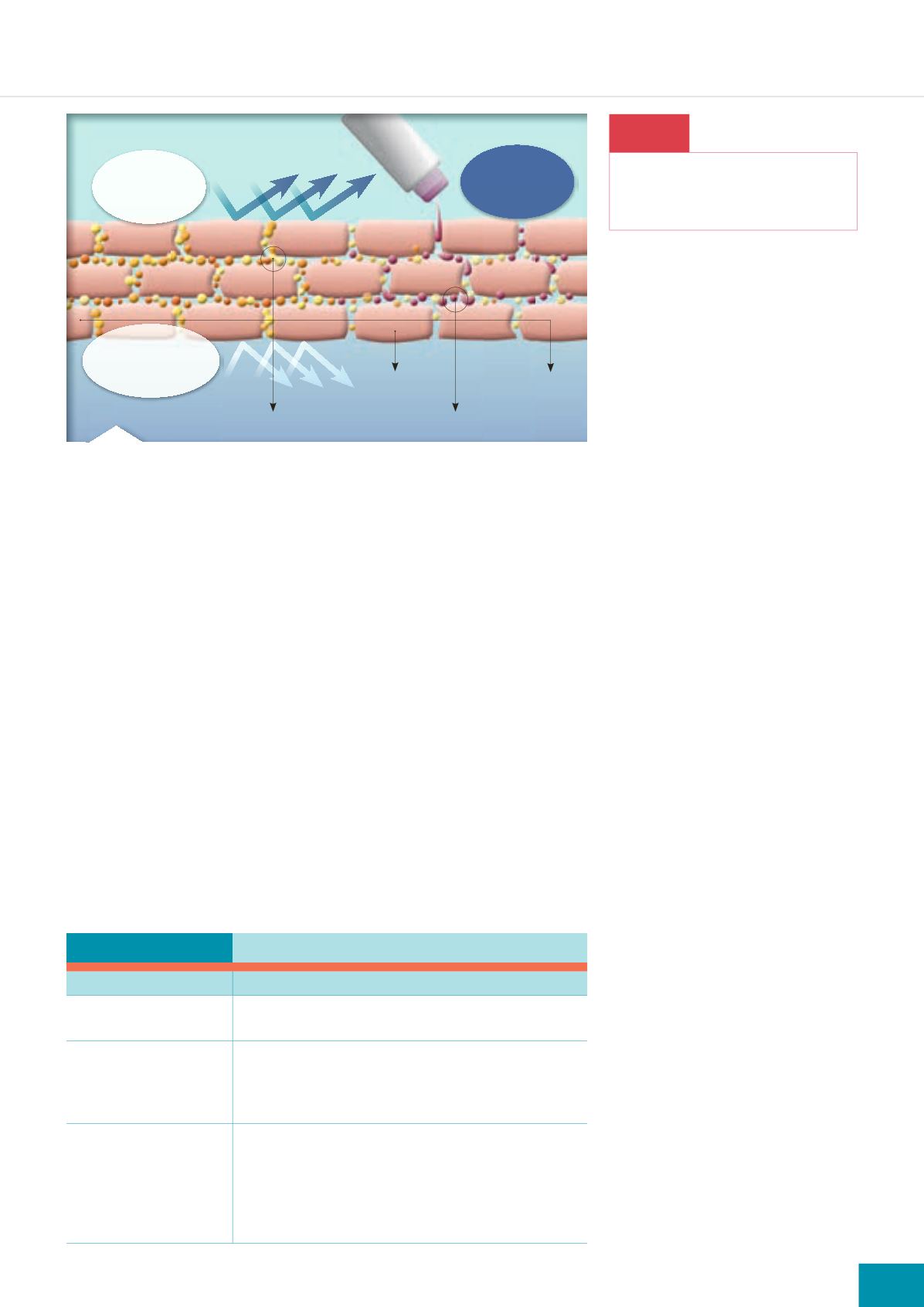
Table 3:
Stepped management of atopic eczema (NICE, 2007)
Severity
Management
Mild
i
Emollient therapy (creams, lotions and ointments)
i
Topical corticosteroids (mild potency )
Moderate
i
Emollient therapy
i
Topical corticosteroids (moderate potency)
i
Topical calcineurin inhibitors
i
Bandages
Severe
i
Emollient therapy
i
Topical corticosteroids (moderate potency)
i
Topical calcineurin inhibitors
i
Bandages
i
Phototherapy
i
Systemic therapy (immunosuppressant drugs)
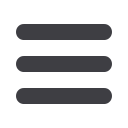
Figure 1.
Mode of action of emollients.
Replenishing
effect
Protection
against
pollutants
Protection against
moisture loss
Horny layer
Horny cell
Epidermal lipids
Emollients