14
WOUND CARE TODAY
2014,Vol 1, No 1
FOCUS ON PRESSURE ULCERS
›
A
ccording to the Declaration
of Rio (2011), pressure
ulcers are a major health
problem affecting millions of people
worldwide. They are attributed to
deteriorating patient health
and quality of life, and can
eventually lead to disability
and/or death.
Pressure ulcers are
categorised using the
European Pressure Ulcer
Advisory Panel/National
Pressure Ulcer Advisory
Panel (EPUAP/NPUAP,
2009) category system
(
Table 1
). Pressure ulcers
most commonly occur on
the sacrum and heel, but
can be found over any bony
prominence and, although more
prevalent in the elderly, can affect
patients of any age, in any care
setting (EPUAP/NPUAP 2009).
INCIDENCE
In the UK, the incidence in
acute care varies between 4%
and 21.9% (Posnett and Franks,
2007; Vanderwee et al, 2007). In
1999/2000, the incidence of pressure
Pressure ulcer prevention: a priority
ulcers in acute medical and surgical
specialities within the UK was
reported as 4%. Excluding mental
illness, learning disability and
obstetric admission, there were 7.95
million admissions during those 12
months. Working on a 4% incidence
of pressure ulcers, a total of 320,000
patients would have developed
pressure ulcers during that time
period (Posnett and Franks, 2007).
The National Patient Safety Agency
(NPSA, 2010) claimed that pressure
ulcers were not only a problem
among the old and ill, but can occur
in any age and in any location.
Indeed, since 2005, they had
received around 100 patient
safety incidents of women
developing pressure ulcers in
maternity wards having given
birth. Furthermore, with an
increasing elderly population,
the problem is inevitably set
to increase (Costa, 2013).
Pressure ulcers are not only
detrimental to patients, they
are also costly for the NHS. An
estimated annual national cost
of pressure ulcer care in the
UK is up to £4 billion, with the
cost of treating the most severe
pressure ulcers ranging from £11,000
to £40,000 per person (NPSA, 2010).
However, the majority of pressure
ulcers are avoidable (Clark, 2007),
with the NPSA (2010) highlighting
Menna Lloyd-Jones, retired senior nurse, tissue
viability, North Wales
IN BRIEF
It is estimated that 95% of all pressure ulcers are preventable.
Development of avoidable pressure ulcers is seen as an indicator
of poor nursing care.
Trusts who fail to prevent avoidable pressure ulcers can incur
financial penalties.
This article discusses the cost and incidence of pressure ulcers, and
the use of care bundles in preventing their development.
KEYWORDS:
Pressure ulcer prevention
Risk assessment
Avoidable and
unavoidable pressure
ulcers
Care bundles
Menna Lloyd-Jones
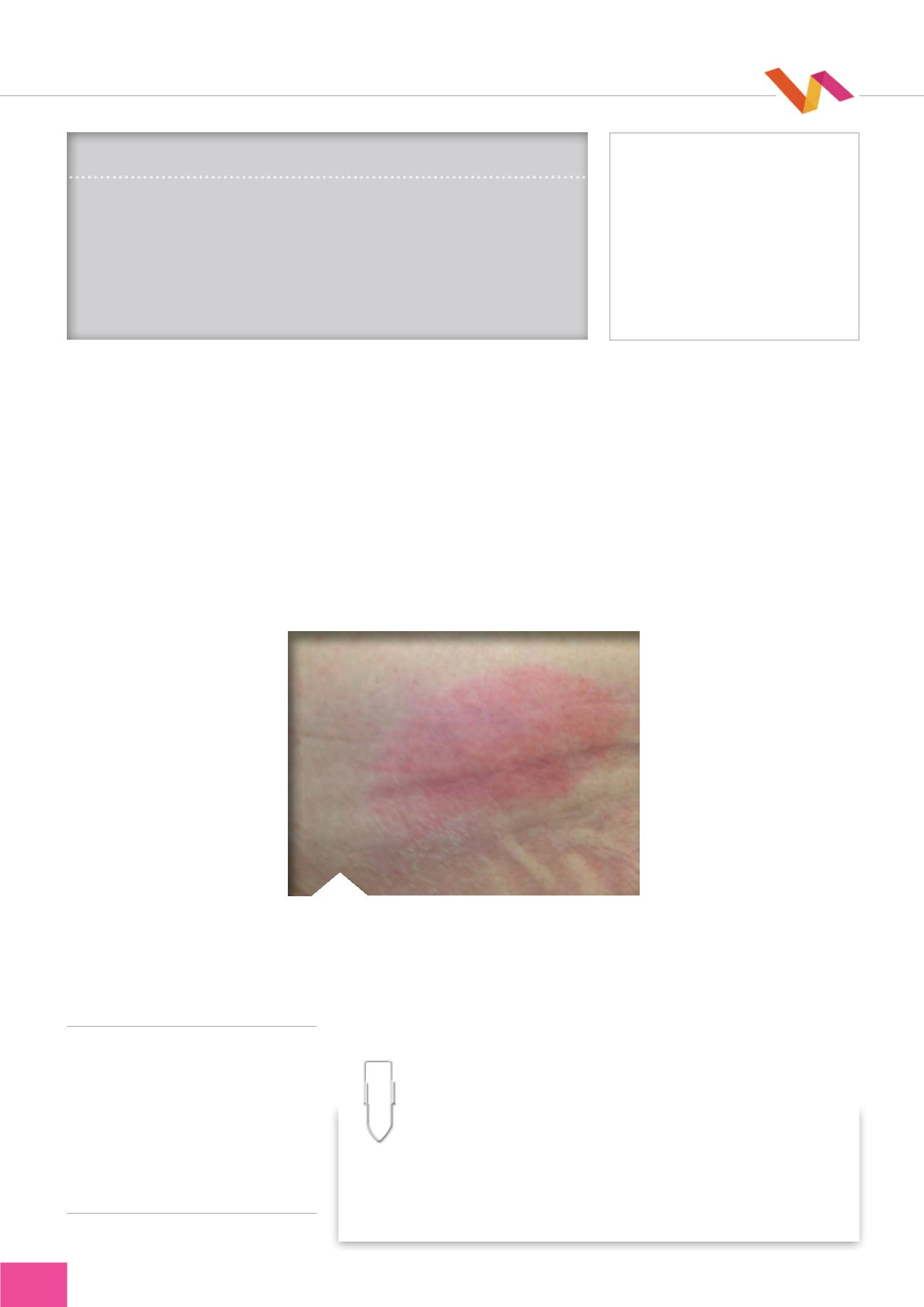
Figure 1.
Category 1 pressure ulcer.
THE SCIENCE
A pressure ulcer is defined as localised injury to the skin and
underlying tissue usually over a bony prominence, as a result of
pressure, or pressure in combination with shear. A number of contributing
or confounding factors are also associated with pressure ulcers, although
significance of these is yet to be elucidated (EPUAP/NPUAP, 2009).